Perimenopause and Sleep: The Surprising Truth Behind Your Restless Nights After 40

As we journey into our 40s, the quality and pattern of our sleep often undergoes significant changes. Research shows that 40-70% of adults over 40 experience regular sleep disturbances, with women being particularly affected during perimenopause and menopause. If you’ve noticed you’re waking up more frequently, falling asleep earlier, or feeling less rested, you’re experiencing a natural biological shift – one that can be effectively managed with the right approach.
In this comprehensive guide, we’ll explore the science behind these mid-life sleep changes and provide practical, evidence-based strategies to help you adapt and reclaim restful nights.
📺 **Watch Short version Now: Perimenopause and Sleep: How Hormonal Changes Affect Your Rest After 40 **
Perimenopause and Sleep: Related Changes in Sleep Architecture After 40
Between 40% and 70% of older adults face ongoing sleep disturbances, and doctors leave half these cases undiagnosed. The natural connection between perimenopause, sleep and aging surprises many people, especially the changes that emerge after 40. As we explore sleep changes with age, it’s important to understand how our bodies adapt over time.
Your sleep patterns undergo the most important changes gradually. The body shifts toward lighter sleep phases instead of deep, restful ones. Research shows our bodies produce less melatonin with age, which causes frequent wake-ups at night and earlier rising times. These disruptions can trigger serious health risks – from heart disease to memory issues and drowsiness during the day.
This piece explores the science behind sleep changes after 40 and provides solutions to address them effectively. You’ll discover practical ways to adapt to your changing sleep needs and enhance your rest quality, whether you’re nearing forty or already past it, including strategies to increase deep sleep in elderly individuals.
Perimenopause and Sleep Issues: The Hormonal Connection
The way hormones and sleep interact becomes clearer as we reach 40. Our bodies go through subtle yet deep biological changes that affect how we rest at night, impacting various aspects of sleep, including sleep onset latency and overall sleep efficiency.
The transition to menopause (perimenopause) brings significant hormonal fluctuations that directly impact sleep quality. Research shows that 56% of perimenopausal women sleep less than seven hours nightly, and 24.8% report trouble falling asleep four or more times weekly.
The Hormonal Mechanism Behind Sleep Disruption
During perimenopause, two key hormones – estrogen and progesterone – undergo dramatic changes:
- Estrogen decline: Estrogen helps regulate body temperature and promotes serotonin production (a precursor to melatonin). As levels fluctuate and decline, hot flashes, night sweats, and reduced melatonin can significantly disrupt sleep.
- Progesterone reduction: This hormone has natural sedative effects. As progesterone levels drop, you may experience more difficulty falling and staying asleep.
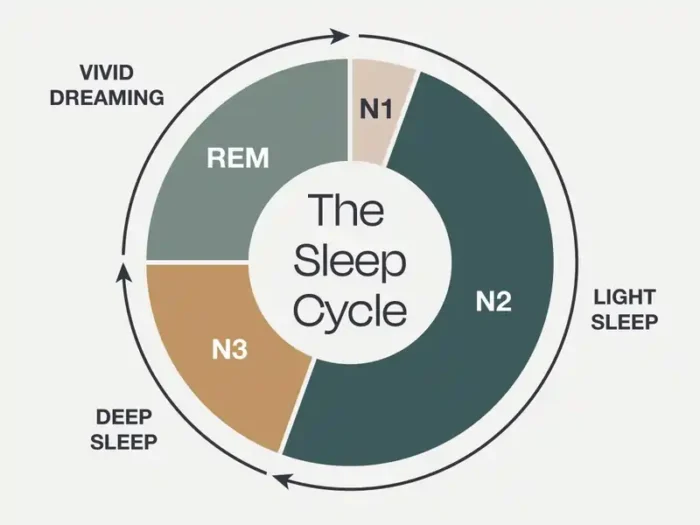
These hormonal shifts don’t just make it harder to fall asleep – they fundamentally alter your sleep architecture by:
- Reducing time spent in restorative deep sleep
- Increasing nighttime awakenings
- Disrupting REM sleep, which affects memory consolidation and emotional processing
For many women, these changes first appear in their early to mid-40s, often before other noticeable signs of perimenopause emerge.
How hormones reshape your sleep architecture
The body’s hormone system starts changing gradually after 40 and reshapes sleep patterns. The hormone balance that helped us sleep well begins to change. This affects both sleep quality and how long we sleep, often leading to insomnia and other sleep disturbances.
Women experience major hormone changes during perimenopause and menopause. Their estrogen and progesterone levels drop, making it harder to sleep well. These changes lead to hot flashes that often wake them up at night [1]. Perimenopause and sleep problems can be particularly challenging, as the body transitions through this phase.
Men face these challenges too. Their testosterone levels decrease with age and disrupt sleep. Both men and women see changes in stress hormones. Research shows evening cortisol levels go up by about 19.3 nmol/L every decade after 50 [2]. High cortisol makes it tough to relax before bed.
These hormone changes affect sleep in several ways:
More frequent wake-ups during the night
Less time spent actually sleeping
Changes in when we feel sleepy and alert
Less deep sleep throughout the night
The natural decline in melatonin secretion
The biggest hormone change affecting sleep comes from reduced melatonin secretion—our sleep hormone. Most people’s melatonin stays stable until about age 40 [3]. The levels start dropping steadily after that.
This drop becomes dramatic over time. People at age 90 produce less than 20% of the melatonin young adults make [3]. This explains why older adults often go to bed earlier, wake up sooner, and have trouble staying asleep. The relationship between melatonin and menopause is complex, with some women finding melatonin supplements helpful for managing sleep issues during this transition.
Age brings several reasons for lower melatonin. The pineal gland that makes melatonin often develops calcium deposits [3]. Eye problems like cataracts make it harder to sense light properly, which throws off melatonin production [3].
Changes in growth hormone and deep sleep connection
Growth hormone production changes significantly too. While we often link it to childhood growth, this hormone helps repair tissues and regenerate cells in adults.
Young adults produce 60-70% of their daily growth hormone during early sleep, especially during slow wave sleep [2]. This pattern changes with age. Deep sleep drops from about 18.9% in early adulthood (16-25 years) to just 3.4% in midlife (36-50 years) [2].
Growth hormone levels then drop sharply—about 372 μg every decade from young adulthood to middle age [2]. The decline slows later to roughly 43 μg per decade [2].
This creates a two-way effect: less deep sleep reduces growth hormone, and lower growth hormone affects sleep quality. This cycle becomes harder to break as we get older, contributing to the overall changes in sleep stages by age.
Learning about these biological changes helps us adapt our sleep habits. We can work with our changing biology instead of fighting it to get better rest.
“Hormonal fluctuations during perimenopause don’t just affect sleep onset – they fundamentally alter sleep architecture by reducing time spent in deep, restorative sleep stages and increasing nocturnal awakenings.” — Dr. Sara Mednick, Professor of Cognitive Science, University of California
How Perimenopause Affects Sleep Quality in Your 40s
The transition to menopause (perimenopause) brings significant hormonal fluctuations that directly impact sleep quality. Research shows that 56% of perimenopausal women sleep less than seven hours nightly, and 24.8% report trouble falling asleep four or more times weekly.
The Hormonal Mechanism Behind Sleep Disruption
During perimenopause, two key hormones – estrogen and progesterone – undergo dramatic changes:
- Estrogen decline: Estrogen helps regulate body temperature and promotes serotonin production (a precursor to melatonin). As levels fluctuate and decline, hot flashes, night sweats, and reduced melatonin can significantly disrupt sleep.
- Progesterone reduction: This hormone has natural sedative effects. As progesterone levels drop, you may experience more difficulty falling and staying asleep.
These hormonal shifts don’t just make it harder to fall asleep – they fundamentally alter your sleep architecture by:
- Reducing time spent in restorative deep sleep
- Increasing nighttime awakenings
- Disrupting REM sleep, which affects memory consolidation and emotional processing
For many women, these changes first appear in their early to mid-40s, often before other noticeable signs of perimenopause emerge.
How Your Sleep Stages Shift With Age
“Sleep comes more easily than it returns.” — Victor Hugo, French poet, novelist, and dramatist
Sleep architecture—the way our sleep stages flow throughout the night—changes dramatically as we age. These changes go beyond just sleeping less. Your brain cycles through different types of sleep in fundamentally different ways, affecting overall sleep efficiency by age.
Less deep sleep, more light sleep: what it all means
The brain’s sleep patterns start changing early in adult life. Research shows deep slow wave sleep (our most restorative sleep stage) drops from 18.9% during early adulthood (ages 16-25) to only 3.4% by midlife (ages 36-50) [2]. Most people don’t even notice these changes happening.
This missing deep sleep doesn’t just vanish—lighter sleep stages take its place. Light NREM sleep (stages 1 and 2) rises from 51.2% in early adulthood to 67.3% by midlife [2]. Your brain spends more time in shallow sleep and less time in deeply refreshing stages.
Deep sleep matters because your body uses this time to perform vital maintenance:
Physical restoration and tissue repair
Memory consolidation
Immune system strengthening
You might feel less refreshed in the morning with reduced deep sleep, even after spending the same time in bed. These changes happen regardless of sleep disorders or health conditions.
REM sleep alterations after midlife
REM sleep (when we typically dream) stays stable until about age 50, unlike deep sleep which drops sharply by midlife. After 50, REM sleep starts declining by about 10 minutes every decade [2].
Studies show REM sleep decreases about 0.6% per decade from age 19 to 75 [4]. Some research points to a small uptick in REM sleep between ages 75 and 85, but the overall trend points downward [4].
REM sleep changes can impact your brain’s function because this stage plays vital roles in:
Emotional regulation
Creative thinking
Memory processing
Research suggests REM sleep quality could signal early cognitive decline risk in healthy older adults [5].
Why you wake up more frequently at night
Waking up throughout the night becomes more common with age. The time spent awake increases by about 28 minutes per decade from midlife to late life [2]. This mostly affects light non-REM sleep (down 24 minutes per decade) and REM sleep (down 10 minutes per decade) [2].
Several factors cause these nighttime awakenings:
Your sleep naturally becomes more fragmented with age, leading to more brief wake-ups throughout the night. Brief awakenings increase steadily between ages 30 and 60 [4].
The brain’s ability to keep muscles still during REM sleep weakens over time, which can disrupt sleep [6].
Your body becomes less efficient at staying asleep, leading to longer periods of wakefulness after sleep onset (WASO). Between ages 30 and 60, WASO increases by about 10 minutes every decade [4].
All the same, not every sleep change continues forever. Many sleep patterns, including WASO and deep sleep percentage, tend to level off after age 60 [4]. While sleep changes substantially from young adulthood to midlife, it often finds a new balance in later years.
Table: Sleep Stage Changes
| Sleep Metric | Young Adult (20-30) | Midlife (40-50) | Impact |
|---|---|---|---|
| Deep Sleep % | 18.9% | 3.4% | Reduced cellular repair, memory consolidation |
| REM Sleep % | 23-25% | 18-20% | Decreased emotional processing, creativity |
| Sleep Efficiency | 95% | 85% | More time awake during night |
| Nighttime Awakenings | 2-3 | 5-7 | Fragmented sleep, reduced restorative benefit |
Menopause and Insomnia: Why It Happens and What Helps
Your body clock goes through a gradual yet radical alteration when you turn 40. The change in your circadian rhythm—your 24-hour biological cycle—helps explain why your sleep patterns might feel different.
Why you get sleepy earlier and wake up earlier
Late-night TV becomes a struggle to stay awake and suddenly you’re wide awake at 5 AM. This isn’t just a habit you’ve picked up—your biology makes it happen. Your circadian rhythm starts moving earlier around age 40, and this pattern becomes stronger each decade.
Scientists call this “phase advance.” Your body naturally wants to sleep earlier in the evening and wake up earlier in the morning [7]. The body runs on an earlier schedule now, whatever your social life or previous routines might be.
People in their 60s typically experience their circadian timing about one hour earlier compared to their younger days [4]. Research reveals something fascinating – many older adults’ internal body clocks naturally want them to sleep around 7-8 PM and wake up at 3-4 AM [7]. Social schedules rarely match this biological need.
This creates some real problems. The body clock still triggers an early morning wake-up around 3-4 AM even when older adults try staying up late. This leads to disrupted sleep afterward [7].
The science of circadian rhythm shifts
Your brain’s master timekeeper, a tiny cluster of cells called the suprachiasmatic nucleus (SCN), controls these changes [8]. This internal clock sits in the hypothalamus and coordinates almost all your daily biological rhythms.
Age affects how the SCN works in several ways:
The aging process reduces light entering your eyes, especially the short-wavelength blue light that regulates your circadian rhythm [7]. The SCN becomes less sensitive to light signals [4]. The molecular machinery inside the SCN loses its rhythmic power [9].
These changes combine with decreased melatonin secretion to create a more sensitive timing system. Scientists have discovered that older adults need to sleep within specific time windows to get proper rest [7].
This timing adjustment affects your brain power too. Morning cognitive tests show older adults performing as well as younger people, but their performance drops in afternoon testing [10]. Jet lag recovery and shift work adaptation become tougher with age [4].
Better sleep quality comes from working with these natural changes in your body clock instead of fighting them.
Why Elderly Have Trouble Sleeping: Changes in Sleep Architecture
Sleep patterns naturally change as we age, but midlife brings additional challenges that can make rest even more difficult. People dealing with sleep and aging issues should understand these common sleep disruptors, including those related to menopause insomnia, perimenopause and sleep problems.
Physical factors: pain, temperature regulation, and bathroom trips
The body becomes more sensitive to discomfort after 40. Poor sleep and chronic pain go hand in hand in 90% of cases, each making the other worse. People with back pain often find their discomfort gets worse the day after a bad night’s sleep.
Body temperature control becomes a major challenge, especially during menopause. Hot flashes interrupt sleep for 40-60% of women going through menopause, often causing unexpected wake-ups. Research points to an interesting finding – waking up might actually trigger hot flashes rather than the other way around. Some women find that melatonin supplements can help with night sweats, though the relationship between melatonin and hot flashes is still being studied.
Nighttime bathroom visits increase with age because bladder function changes and hormone production decreases.
“After 40, the brain produces less delta waves during deep sleep, which directly impacts memory consolidation and cellular repair. This explains why many people find their sleep feels less refreshing, even when getting the same number of hours.” — Dr. Matthew Walker, Professor of Neuroscience and Psychology, UC Berkeley
Psychological factors: stress, anxiety, and life transitions
Major life changes often happen during midlife. Children leaving home, career changes, and relationship shifts create mental stress that affects sleep quality. Many people feel lonely as they get older, which leads to insomnia symptoms through increased stress and heightened watchfulness.
Mental health struggles become more common during this time – about 40% of people with insomnia also have a mental health disorder. This creates a difficult cycle where poor sleep affects mood and mood problems disturb sleep even more.
Medical conditions that emerge in midlife
Sleep disorders become more common during these years. Sleep apnea risk rises sharply – women after menopause are two to three times more likely to develop it compared to those before menopause. Restless legs syndrome is another condition that can significantly impact sleep quality in middle-aged and older adults.
The body’s hormone changes after menopause affect sleep patterns and overall health. Women who experience moderate-to-severe hot flashes are almost three times more likely to wake up frequently at night. Menopause insomnia can be particularly challenging, with many women wondering about its duration and seeking relief.
Type 2 diabetes, heart disease, and digestive problems commonly develop in midlife. These conditions can disrupt sleep by increasing inflammation throughout the body.
Related post: How To Get Better Sleep
Science-Backed Solutions for Better Sleep After 40
“Eating the right foods provides energy for your workout and improves the quality of your sleep. In turn, a sound night of sleep makes you more likely to eat right the next day. This is why the real magic lies at the intersection between eating, moving, and sleeping. If you can do all three well, it will improve your daily energy and your odds of living a long, healthy life.” — Tom Rath, Author and researcher
Sleep quality doesn’t have to decline with age. Research shows several strategies that work well for midlife sleep challenges, including ways to increase deep sleep in elderly individuals.
Timing techniques to work with your changing body clock
Your body’s natural rhythms work best when you cooperate with them. Studies show you can reset your circadian rhythms by adjusting your schedule gradually – no more than an hour each day [11]. This prevents the collateral damage that comes from sudden changes. A regular sleep schedule matters most. Your internal clock becomes stronger when you stick to the same sleep-wake times, even on weekends.
Getting morning sunlight right after waking helps shift your circadian rhythms earlier. This helps if you feel sleepy too early in the evening [11]. Your meal times can also change your body clock. Eating breakfast as soon as you wake up helps advance your sleep schedule [11].
Environment optimization for deeper sleep
The right bedroom setup makes a huge difference in sleep quality. Your bedroom should be as dark as possible – even small amounts of light can disrupt melatonin secretion [11]. Temperature plays a crucial role too. Sleep experts say rooms between 65-68°F work best [12].
Sound machines or earplugs help reduce the frequent sleep disturbances common after 40 [12]. Your brain makes stronger connections between your bed and rest when you use your bedroom only for sleep and sex [12].
Nutrition and exercise approaches that work
Daily exercise substantially improves sleep quality. Research shows people who exercise at least 30 minutes daily sleep about 15 minutes longer than those who don’t [3]. The timing of your workout matters. Morning or early afternoon exercise helps you sleep better, but working out too close to bedtime might keep you awake [13].
Your evening habits affect sleep quality too. Cutting back on caffeine and alcohol helps prevent sleep disruption [14]. Light evening meals help you avoid digestive issues that interfere with rest [12].
When to think over sleep aids and supplements
Some supplements might help with ongoing sleep issues. Melatonin helps you fall asleep faster and sleep longer. This works especially well for adults over 40 who naturally produce less melatonin [15]. Small doses work best – try 0.5-1mg about 30 minutes before bed [16]. For those dealing with perimenopause and sleep issues, melatonin for perimenopause can be particularly beneficial.
Magnesium supplements might improve your sleep by relaxing muscles and helping regulate melatonin secretion [15]. Stress-related sleep problems often respond well to adaptogens like ashwagandha, which help normalize your body’s stress response [16].
For persistent insomnia, especially related to menopause or aging, cognitive behavioral therapy for insomnia (CBT-I) has shown promising results. This non-pharmacological approach can help address the underlying causes of sleep disturbances and improve overall sleep quality.
Sleep and Metabolic Health: The Connection After 40
The relationship between sleep and metabolism becomes particularly significant after 40, when metabolic rate naturally begins to slow.
How Poor Sleep Affects Your Metabolism
Research reveals that sleep deprivation leads to consuming an average of 285 additional calories daily – equivalent to gaining nearly 30 pounds annually if not balanced with increased activity. This occurs through several mechanisms:
- Hormonal disruption: Poor sleep elevates cortisol (stress hormone) while disrupting hunger hormones – increasing ghrelin (which stimulates appetite) and decreasing leptin (which signals fullness).
- Insulin resistance: Just one night of inadequate sleep can reduce insulin sensitivity by 25%, increasing blood sugar fluctuations and energy crashes that prompt carbohydrate cravings.
- Muscle preservation: Deep sleep stages trigger growth hormone release, which maintains muscle mass – crucial for maintaining metabolic rate after 40 when natural muscle loss accelerates.
Metabolic-Friendly Sleep Strategies
Balance blood sugar before bed: Avoid high-carbohydrate evening meals that can trigger nighttime hot flashes and sleep disruptions through blood sugar fluctuations.
Maintain consistent meal timing: Eating dinner at least 3 hours before bedtime helps prevent disruptions to deep sleep.
Consider protein timing: A small protein snack (10-15g) 30 minutes before bed can help stabilize blood sugar and provide tryptophan, a precursor to melatonin.
Monitor caffeine clearance: After 40, the liver often metabolizes caffeine more slowly. Try cutting off caffeine intake by 2pm instead of the commonly recommended 4pm.
Gender Differences in Midlife Sleep Patterns
While both men and women experience age-related sleep changes after 40, the underlying mechanisms and manifestations differ significantly.
Men’s Sleep Changes After 40
Men face their own hormonal transitions that impact sleep quality:
- Testosterone decline: Starting around age 40, testosterone levels decrease approximately 1-2% annually. This gradual reduction, sometimes called “andropause,” can negatively affect sleep quality and increase susceptibility to sleep apnea.
- Sleep apnea risk: Men are 2-3 times more likely than premenopausal women to develop obstructive sleep apnea, with risk increasing significantly after 40. Signs include loud snoring, gasping during sleep, and excessive daytime fatigue.
- Prostate changes: Enlarged prostate (BPH) becomes increasingly common after 40, leading to nocturia (nighttime urination) that disrupts sleep continuity.
Women’s Sleep Changes After 40
Women’s sleep experiences are heavily influenced by reproductive hormonal shifts:
- Vasomotor symptoms: Hot flashes and night sweats affect up to 80% of women during perimenopause and can persist for 7+ years, causing frequent night awakening.
- Mood disturbances: Hormonal fluctuations increase susceptibility to anxiety and depression, which have bidirectional relationships with sleep disruption.
- Protective factors loss: Prior to perimenopause, women typically have more deep sleep and better sleep efficiency than men – advantages that diminish during the menopausal transition.
Gender-Specific Sleep Strategies
For men:
- Regular screening for sleep apnea, especially if experiencing daytime fatigue
- Maintaining healthy weight to reduce apnea risk
- Limiting evening fluids to reduce nighttime awakenings from prostate issues
For women:
Consistent sleep/wake schedule to stabilize irregular hormonal patterns
Cooling strategies for nighttime hot flashes (moisture-wicking sleepwear, bedroom temperature 65-68°F)
Stress management techniques to address heightened anxiety effects on sleep
How Modern Technology Affects Sleep After 40
As we age, our sensitivity to blue light emitted from screens increases. Research shows that adults over 40 experience up to 37% more melatonin suppression from evening screen exposure compared to younger adults.
The Double Threat of Digital Devices After 40
- Enhanced Blue Light Sensitivity: After 40, the crystalline lens in your eye begins to yellow, paradoxically making you more sensitive to blue light which suppresses melatonin production.
- Slower Circadian Recovery: Your body’s ability to reset its circadian rhythm after disruption decreases by approximately 30% each decade after 40, making consistent digital habits crucial.
Digital Wellness Strategies for Midlife Sleep
Position Screens Properly: Keep screens at least 18-24 inches from your face and slightly below eye level to reduce neck strain that compounds age-related muscle tension affecting sleep quality.
Implement the 10-10-10 Rule: No screens 10 minutes after waking, 10 minutes before meetings (to prevent stress spikes), and 10 hours before your intended wake-up time (usually 1-2 hours before sleep).
Use Night Mode Plus: Standard night mode reduces blue light by ~20%, but people over 40 benefit from maximum settings and additional blue light glasses, which together can preserve up to 95% of natural melatonin production.
Common Sleep Disorders After 40: When to Seek Help
While some sleep changes are normal aging processes, certain conditions require medical attention. Here’s how to distinguish normal changes from sleep disorders that emerge in midlife:
Sleep Apnea: The Hidden Midlife Risk
Sleep apnea risk increases dramatically after 40, with prevalence rates jumping from 2-4% in younger adults to 17-24% in midlife. Men are particularly vulnerable as throat muscles lose tone and weight distribution shifts toward the upper body.
Warning signs that distinguish sleep apnea from normal aging:
- Gasping or choking sensations that wake you
- Morning headaches that weren’t previously common
- Extreme daytime fatigue despite 7-8 hours in bed
- Witnessed breathing pauses (reported by a partner)
When to see a doctor: If you experience any of the warning signs above, especially if you have risk factors such as being male, over 40, or having a BMI over 25.
Insomnia: Normal Disruption vs. Clinical Issue
While 92% of adults over 40 report occasional sleep difficulties, clinical insomnia affects about 35%. The distinction lies in frequency and impact:
Normal midlife sleep changes:
- Taking 15-25 minutes to fall asleep
- 1-2 brief awakenings per night
- Occasional difficult nights during stressful periods
Clinical insomnia requiring treatment:
Daytime functioning significantly impaired
Taking more than 30 minutes to fall asleep at least 3 nights weekly
Awakening for more than 30 minutes at least 3 nights weekly
Personalized Sleep Solutions: Finding What Works for You
Sleep needs and challenges evolve throughout your 40s and 50s. Use this self-assessment to identify your specific sleep profile and targeted solutions:
Quick Sleep Profile Self-Assessment
Answer these questions to identify your primary sleep challenge:
- Do you have trouble falling asleep initially? (Yes/No)
- Do you wake frequently during the night? (Yes/No)
- Do you wake too early and can’t return to sleep? (Yes/No)
- Do you sleep a sufficient amount but still feel unrefreshed? (Yes/No)
Tailored Solutions By Age and Sleep Challenge
Early 40s (40-44) – Primary Challenge: Falling Asleep
- Biological shift: Cortisol patterns begin changing
- Targeted solution: Time-restricted eating (finish dinner by 7pm)
- Supplement focus: Magnesium glycinate (300-400mg)
- Environmental adjustment: Reduce ambient temperature to 65-67°F
Mid-40s (45-49) – Primary Challenge: Nighttime Awakenings
Environmental adjustment: White noise machine calibrated to specific frequencies that benefit midlife sleep architecture
Biological shift: Significant hormonal fluctuations (perimenopause/testosterone decline)
Targeted solution: Split-sleep schedule (20-minute afternoon nap, 7-hour main sleep)
Supplement focus: Adaptogenic herbs (ashwagandha, rhodiola)
Related post: Perfect Night Routine
Comparative Table for Age-Related Sleep Changes
| Age Group | Average Sleep Duration | Common Sleep Issues | Recommended Solutions |
| 20s-30s | 7-9 hours | Work stress, technology use | Digital curfew, consistent schedule |
| 40s-50s | 7-8 hours | Perimenopause, stress | Hormone-balancing activities, temperature regulation |
| 60s+ | 7-8 hours | Early waking, less deep sleep | Light exposure management, sleep consolidation techniques |
Trusted Resources:
National Institute on Aging: www.nia.nih.gov/health/good-nights-sleep
Sleep Foundation: www.sleepfoundation.org/aging-and-sleep
Cleveland Clinic: health.clevelandclinic.org/sleep-changes-in-older-adults
Conclusion
Sleep changes after 40 are a natural biological change, not a disorder. These changes might feel frustrating at first, but knowing the science behind them helps us adapt better.
Research shows our sleep patterns change by a lot during midlife. Your body makes less melatonin and your internal clock starts to work differently. On top of that, physical and mental factors at this age can affect how well you rest. All the same, you don’t have to accept poor sleep as unavoidable.
Science gives us many ways to sleep better after 40. Regular sleep schedules, a better bedroom setup, and the right exercise timing can improve your rest quality. While melatonin supplements might help some people, changing your daily habits works best for better sleep in the long run.
Your best approach is to work with these age-related changes instead of fighting them. Small tweaks like going to bed earlier and getting morning sunlight can arrange your habits with your body’s natural patterns. Note that everyone goes through these changes, which helps us handle them with more patience and understanding.
FAQs
How does sleep typically change after 40?
Sleep patterns often shift as we age, with many people experiencing earlier bedtimes, more frequent nighttime awakenings, and less deep sleep. These changes are largely due to natural biological shifts in our sleep architecture and circadian rhythms.
Why do I wake up more frequently during the night as I get older?
Increased nighttime awakenings are common after 40 due to several factors, including changes in sleep architecture, decreased melatonin secretion, and physical discomforts like pain or the need for bathroom trips. This fragmentation of sleep is a normal part of aging.
Can hormonal changes affect sleep during midlife?
Yes, hormonal fluctuations, particularly during perimenopause and menopause, can significantly impact sleep. Changes in estrogen and progesterone levels can lead to sleep disturbances, night sweats, and alterations in sleep patterns. Many women wonder, “Does menopause affect sleep?” and the answer is a resounding yes.
What are some effective strategies for improving sleep quality after 40?
To enhance sleep quality, maintain a consistent sleep schedule, create a comfortable sleep environment, engage in regular exercise (but not too close to bedtime), limit caffeine and alcohol intake, and expose yourself to morning sunlight. These strategies can help align your habits with your body’s changing rhythms and improve overall sleep efficiency.
Should I consider using sleep aids or supplements as I age?
While lifestyle modifications are often most effective for long-term sleep improvement, some supplements may help. Melatonin can be beneficial for reducing sleep onset latency, especially as natural melatonin production declines with age. For those dealing with menopause-related sleep issues, a specific melatonin dosage for menopause may be recommended. However, it’s always best to consult with a healthcare professional before starting any new supplement regimen.
References
[1] – https://www.sleep.com/sleep-health/sleep-when-youre-middle-aged
[2] – https://jamanetwork.com/journals/jama/fullarticle/192981
[3] – https://pmc.ncbi.nlm.nih.gov/articles/PMC10503965/
[4] – https://pmc.ncbi.nlm.nih.gov/articles/PMC5841578/
[5] – https://www.nature.com/articles/s42003-024-06415-y
[6] – https://sleep.hms.harvard.edu/education-training/public-education/sleep-and-health-education-program/sleep-health-education-79
[7] – https://www.sleepfoundation.org/circadian-rhythm/how-age-affects-your-circadian-rhythm
[8] – https://my.clevelandclinic.org/health/articles/circadian-rhythm
[9] – https://www.nature.com/articles/s41467-021-22922-6
[10] – https://pmc.ncbi.nlm.nih.gov/articles/PMC5272178/
[11] – https://www.sleepfoundation.org/circadian-rhythm/can-you-change-your-circadian-rhythm
[12] – https://www.sleepfoundation.org/sleep-hygiene/healthy-sleep-tips
[13] – https://www.hopkinsmedicine.org/health/wellness-and-prevention/exercising-for-better-sleep
[14] – https://www.bphope.com/bipolar-buzz/9-ways-to-reset-your-body-clock-for-better-sleep/
[15] – https://www.healthline.com/nutrition/sleep-aids
[16] – https://drannagarrett.com/sleep-supplements-for-perimenopause/