Sleep Apnea and Aging: The Hidden Connection to Accelerated Aging

Sleep apnea and aging connection is nowhere near as simple as most people think. Approximately 22 million Americans struggle with sleep apnea. This condition affects roughly 1 in 15 adults, and many cases remain undiagnosed.
My experience as a health professional has shown how this common sleep disorder quietly speeds up the aging process.
The numbers paint a stark picture. Each breathing interruption during sleep can add 321 days to your biological age. Research shows that when a person’s apnea-hypopnea index rises by one standard deviation, it adds about 215 days to their biological age.
These findings become even more troubling when you look at obstructive sleep apnea (OSA) rates – 49% of men and 23% of women over age 40 have this condition.
Age plays a crucial role in how sleep apnea affects our bodies. Young adults with severe sleep apnea face higher death risks, yet older adults sometimes show a protective effect against mortality.
This unexpected relationship shows the complex connection between age-related sleep apnea and its effects on our bodies.
The problem goes beyond just feeling exhausted. People under 50 with OSA show specific aging markers, regardless of other health factors.
On top of that, those at high risk of OSA develop carotid plaques more often (15.4%) compared to those without it (9.8%). This shows their blood vessels are aging faster.
In this piece, we’ll explore how sleep apnea speeds up aging, its effects on different age groups, and steps you can take to slow or reverse these changes.
Understanding Sleep Apnea and Aging – Its Prevalence
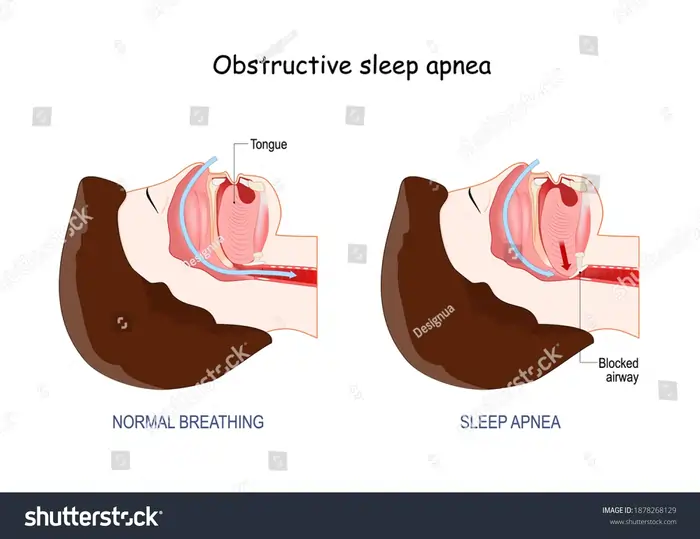
Image Source: Shutterstock
Obstructive sleep apnea is a serious health condition that affects millions worldwide, yet people often overlook it. Let’s get into what OSA is, who it affects most, and why so many people don’t know they have it.
What is obstructive sleep apnea (OSA)?
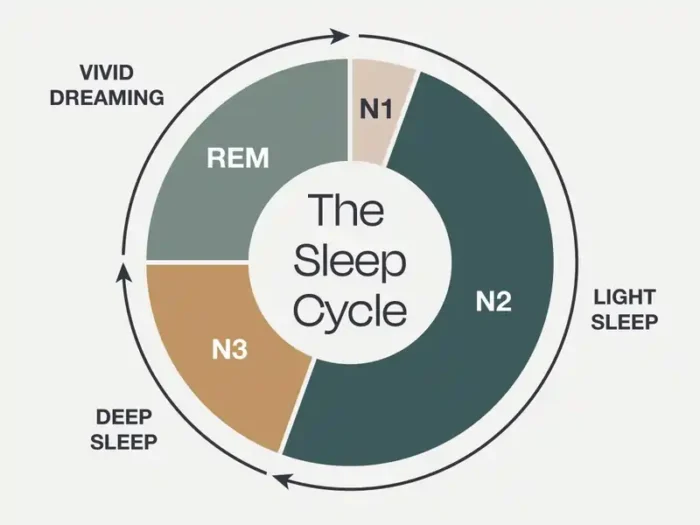
Your throat muscles supporting soft tissues relax while you sleep, and this causes OSA.
Your blood oxygen levels drop during these episodes. Your brain then wakes you up just enough to start breathing again.
Doctors classify OSA severity using the Apnea-Hypopnea Index (AHI), which counts breathing interruptions per hour:
- Mild OSA: AHI between 5-15 events per hour
- Moderate OSA: AHI between 15-30 events per hour
Severe OSA: AHI greater than 30 events per hour
But many mistake their poor sleep quality for normal aging and don’t realize they have a condition.
Sleep apnea prevalence by age and gender
The numbers are staggering worldwide.
Men get OSA more often than women.
Age plays a vital role in OSA development.
Why many cases go undiagnosed
Healthcare providers often lack proper training in sleep disorders.
Without specific questions about sleep problems, patients rarely bring up these issues.
Different populations show different symptoms.
People tend to normalize their symptoms.
Untreated OSA causes more than just poor sleep.
The economic impact is huge—the estimated 23.5 million undiagnosed cases in the US cost about $149.6 billion yearly in healthcare, accidents, and lost productivity.
Resources:
- American Academy of Sleep Medicine: https://aasm.org/
- National Sleep Foundation: https://www.sleepfoundation.org/
- Sleep Research Society: https://www.sleepresearchsociety.org/
Dr. Michael Breus, Clinical Psychologist and Sleep Specialist: “What makes OSA particularly dangerous is that the patient is often unaware of the repeated breathing interruptions during sleep. This silent damage accumulates night after night, accelerating the aging process in multiple body systems before symptoms become obvious.”
How Sleep Apnea Affects the Body
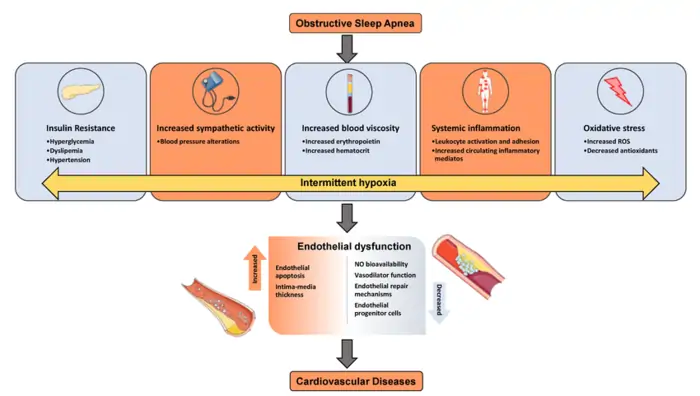
Image Source: ResearchGate
Sleep apnea does more than just ruin your night’s sleep – it frees a cascade of physiological stress throughout the body. The body ages faster through multiple biological pathways every time breathing stops and complex mechanisms kick in.
Intermittent hypoxia and oxygen deprivation
The distinctive pattern of oxygen fluctuations in sleep apnea creates intermittent hypoxia that damages bodily systems. During an apnea episode, oxygen saturation typically drops to 80-85% and returns to normal faster when breathing starts again.
This cyclical pattern of hypoxemia with reoxygenation is different from sustained low-frequency hypoxia.
Tissues experience damage both during oxygen deprivation and, ironically, when oxygen returns.
These cycles happen 9-60 times per hour for 6-12 hours during sleep. This creates a chronic state of oxidative stress that speeds up cellular aging.
Sleep fragmentation and arousals
Sleep apnea wreaks havoc on normal sleep architecture through fragmentation.
Brief arousals cause these disruptions. They happen with each breathing pause and are often too short to remember.
This ongoing fragmentation results in cognitive fatigue and neurocognitive deficits.
Related post: How To Get Better Sleep
Impact on cardiovascular and metabolic systems
Sleep apnea hits the cardiovascular system hardest through several connected mechanisms:
Sympathetic nervous system activation – The chemoreflex triggers with each hypoxic episode and causes sympathetic activation and vasoconstriction .Blood pressure spikes can reach 240/130 mmHg at night .Endothelial dysfunction – OSA patients show higher endothelin levels (a potent vasoconstrictor) and lower nitric oxide levels (a vasodilator).
This creates vascular inflammation and compromised blood vessel function . Systemic inflammation – OSA triggers inflammatory mediators like TNF-α and IL-6 .Constant proinflammatory substances contribute to atherosclerosis development .
Intermittent hypoxia disrupts metabolism just as severely.
Sleep apnea and metabolic dysfunction work both ways.
These physiological stressors – oxygen fluctuations, sleep fragmentation, and cardiovascular/metabolic strain – create ideal conditions to speed up aging. This especially affects vascular health, cognitive function, and metabolic regulation.
Resources:
- American Heart Association: https://www.heart.org/
- National Center for Biotechnology Information: https://www.ncbi.nlm.nih.gov/
- Sleep Foundation: https://www.sleepfoundation.org/
Dr. Susan Redline, Professor of Sleep Medicine at Harvard Medical School: “We’re finding that younger adults with sleep apnea may actually be at higher risk for cardiovascular complications than older adults with the same condition. This challenges our traditional understanding of age-related risks.”
The Concept of Accelerated Aging
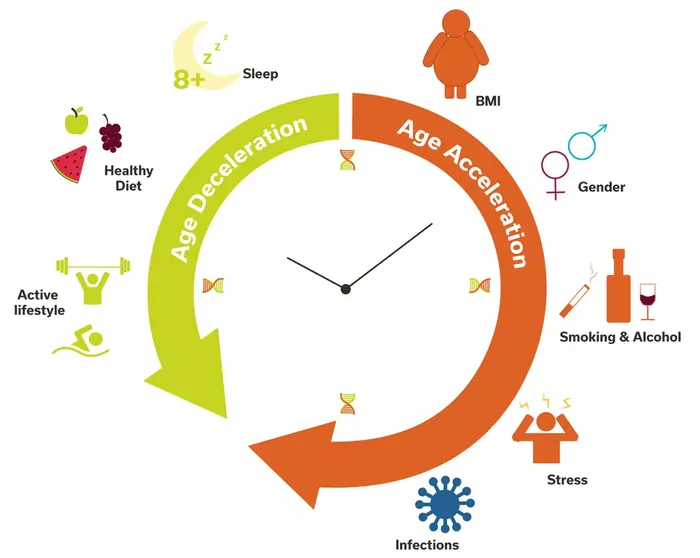
Image Source: Eremid Genomic Services
You need to understand how sleep apnea affects our bodies to see its connection with accelerated aging. This biological deterioration happens faster than our actual age suggests.
Sleep apnea patients often show health problems we typically see in older people.
Chronological vs biological age
Your chronological age counts the years since birth – it’s the same steady progression for everyone.
My patients with the same chronological age often show completely different health profiles.
These biomarkers range from blood pressure readings to molecular markers in cells.
Calendar age associates with disease risk consistently. However, biological age gives us more accurate predictions about health outcomes. This becomes a vital difference for sleep apnea patients because their biological clocks might tick faster than their actual age.
What is epigenetic age acceleration?
Your biological age exceeds your chronological age during epigenetic age acceleration – you age faster than expected. Scientists measure this through DNA methylation.
- First-generation clocks trained on chronological age (Hannum, Horvath)
- Second-generation clocks based on health measures predicting mortality (PhenoAge, GrimAge)
- Third-generation measures like DunedinPACE that estimate actual aging rates
These methylation patterns create predictable signatures that track aging.
Sleep apnea patients face a big challenge here. Their intermittent hypoxia and fragmented sleep create conditions – inflammation, oxidative stress, and metabolic disruption – that can speed up epigenetic aging.
How aging is measured in clinical studies
Scientists use several methods to measure aging beyond chronological markers. Let’s break down how scientists actually measure biological aging.
One fascinating approach uses DNA methylation—think of it as the “software updates” that control how your genetic code is expressed as you age. These methods give precise results but need special lab analysis.
Many studies also use composite scores from routine clinical biomarkers.
Functional assessments give us another way to see biological aging.
New approaches look at aging through specific aging hallmarks – cellular processes that break down over time.
These measurement approaches help explain how sleep apnea might speed up aging. Each interrupted breath does more than just disrupt sleep – it potentially advances biological age through multiple mechanisms that modern science can now measure precisely.
Resources:
- National Institute on Aging: https://www.nia.nih.gov/
- American Academy of Sleep Medicine: https://aasm.org/
- National Center for Biotechnology Information: https://www.ncbi.nlm.nih.gov/
Dr. Rafael Pelayo, Clinical Professor at Stanford Sleep Medicine Center: “The good news is that we now have solid evidence that treating sleep apnea can actually reverse some of the biological aging effects. It’s one of the few medical interventions where we can turn back the clock on certain aging biomarkers.”
Biological Mechanisms Linking OSA to Aging
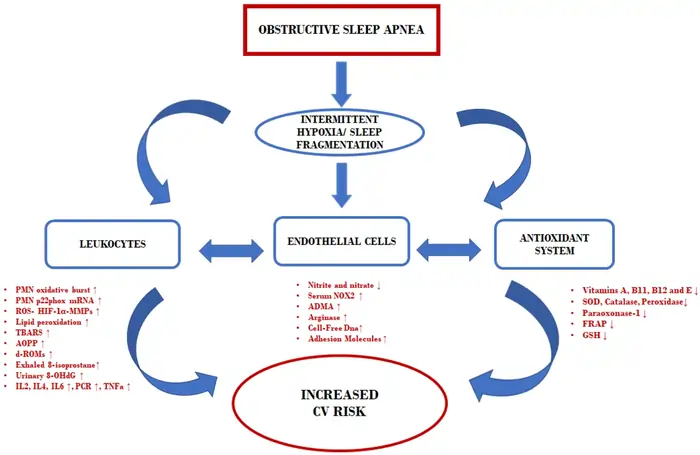
Image Source: MDPI
Sleep apnea speeds up aging at the cellular level through several biological mechanisms.
When breathing patterns break during OSA, they create perfect conditions that harm tissues, change gene expression, and disrupt basic cellular processes. This combination sets the stage for premature aging throughout the body.
Inflammation and oxidative stress
The repeated cycles of hypoxia/reoxygenation in sleep apnea create a severe oxidative imbalance. Breathing stops cause reactive oxygen species (ROS) production to rise while antioxidant defenses weaken. The body experiences chronic oxidative stress that damages cells and tissues.
The oxidative stress-inflammation cycle feeds itself.
Clinical evidence shows that OSA patients have reduced total antioxidant capacity (TAC), which increases oxidative damage.
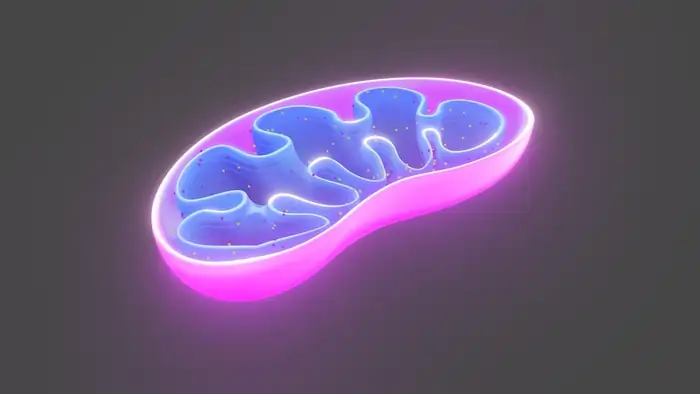
Mitochondrial dysfunction
Sleep apnea affects mitochondria—our cellular powerhouses—particularly hard.
Related post: What Are The Functions of Mitochondria?
Genomic instability and DNA damage
Sleep apnea threatens our cells’ basic blueprint. Lack of oxygen creates oxidative stress that damages DNA and impairs repair mechanisms.
Broken sleep patterns disrupt cell repair that should happen during deep sleep. OSA creates two problems: more DNA damage and less repair ability.
Insulin resistance and nutrient sensing
Sleep apnea substantially disrupts metabolism.
This relationship works both ways—OSA increases diabetes risk while insulin resistance can make sleep apnea worse.
Resources:
- American Academy of Sleep Medicine: https://aasm.org/
- National Institutes of Health: https://www.nih.gov/
- American Diabetes Association: https://diabetes.org/
Gender Differences in OSA’s Aging Effects
While OSA affects men more frequently (34% vs. 17% in women), research suggests women may experience more pronounced accelerated aging effects when they do develop sleep apnea.
Hormonal Influences
Female hormones like estrogen and progesterone help protect breathing regulation during sleep. Post-menopausal women lose this protection, which explains why:
- The gender gap in OSA prevalence narrows after menopause
- Women may experience more severe epigenetic aging effects when OSA develops
Different Symptom Presentation
Women with OSA often report different symptoms than the “classic” presentations:
- Less likely to report loud snoring and witnessed breathing pauses
- More likely to report fatigue, insomnia, and morning headaches
- Often misdiagnosed or attributed to menopause or other conditions
This different symptom profile contributes to underdiagnosis in women, potentially allowing accelerated aging to progress undetected.
Clinical Implications
Healthcare providers should consider gender-specific screening approaches:
- Recognize that standard AHI thresholds may not capture women’s OSA severity accurately
- For women, focus less on snoring and more on fatigue and sleep quality
- Consider OSA testing in post-menopausal women with unexplained fatigue
Vascular Aging and Structural Changes
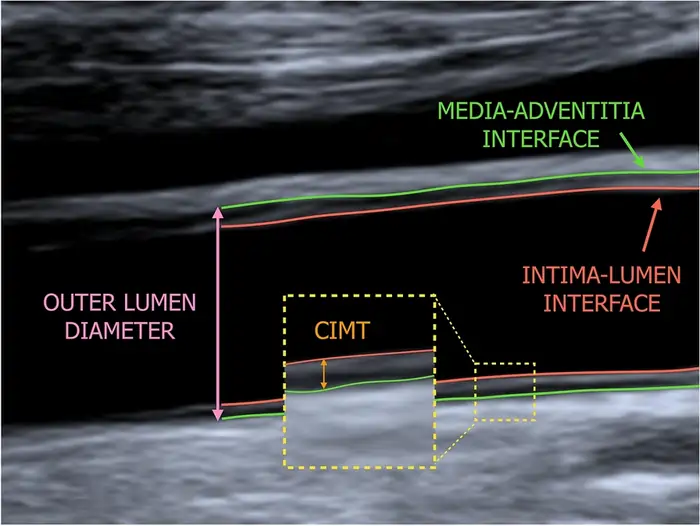
Image Source: link.springer.com
Sleep apnea patients show visible deterioration in their vascular health. Blood vessels provide a vital window to understand how this condition speeds up aging.
Oxygen deprivation and rebound cycles create measurable structural changes that sophisticated imaging and testing methods can detect. These changes provide solid evidence of premature aging in the circulatory system.
Carotid intima-media thickness (IMT)
So how exactly do scientists measure these vascular aging effects? One key method is examining carotid intima-media thickness—a technical term for measuring the thickness of your artery walls.
This measurement reveals the thickness of carotid artery walls—a natural aging process that speeds up under certain conditions.
These findings raise serious concerns.
Pulse wave velocity (PWV)
Imagine blood moving through your arteries like waves. In young, healthy vessels, these waves travel slowly through elastic, flexible tubes. PWV measures exactly how fast these waves move—essentially revealing how stiff your arteries have become.
As we age or develop disease, our arteries lose their elasticity, causing these pressure waves to travel faster. Medical experts consider PWV the “gold-standard” measurement of aortic stiffness because it directly shows how youthful or aged your vascular system really is.
Sleep apnea affects this marker significantly.
Carotid plaques and arterial stiffness
Sleep apnea patients face higher risks of blood vessel structural changes beyond thickened walls and stiff arteries.
Carotid plaques—buildups of lipids, inflammatory cells, and fibrous elements in artery walls—show advanced vascular aging and increased stroke risk.
Research reveals sleep apnea patients develop carotid plaques more often.
Multiple mechanisms drive arterial stiffness in OSA patients.
Hypoxemia seems to affect younger patients more severely.
This highlights the need for early intervention to prevent accelerated vascular aging in younger OSA patients.
Resources:
- American Heart Association: https://www.heart.org/
- National Heart, Lung, and Blood Institute: https://www.nhlbi.nih.gov/
- Sleep Foundation: https://www.sleepfoundation.org/
Age-Specific Effects of Sleep Apnea
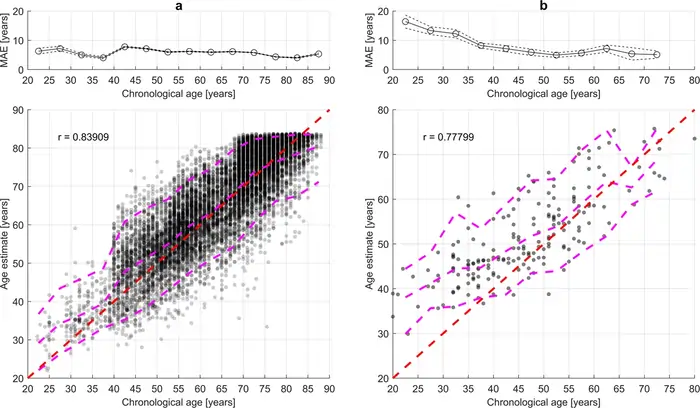
Image Source: Nature
Sleep apnea affects age groups differently, with unexpected patterns between how common it is and its health effects. New research reveals key differences in how obstructive sleep apnea (OSA) affects young and old patients.
Does sleep apnea cause aging more in younger people?
Young adults might age faster when they have sleep apnea.
Older patients only show these changes when they’re awake.
Young OSA patients face bigger heart risks than older ones.
These effects might speed up how fast their bodies age.
Why older adults may show fewer effects
In stark comparison to this, even though more older people have OSA, it affects them less.
This unexpected pattern happens because OSA works differently in older adults.
Sleep apnea death age: what studies show
Death risks from sleep apnea don’t match how common it is.
Research shows that severe OSA raises death risk mostly in patients under 50.
Resources:
- American Academy of Sleep Medicine: https://aasm.org/
- National Institute on Aging: https://www.nia.nih.gov/
- Sleep Research Society: https://www.sleepresearchsociety.org/
Can Aging Itself Cause Sleep Apnea?
Sleep apnea speeds up aging, but here’s another crucial question: Does aging itself cause sleep apnea? Research shows that as our bodies age naturally, we become more likely to develop obstructive sleep apnea (OSA).
Age-related muscle tone loss and airway collapse
Have you ever noticed how an elderly person’s arms or legs look thinner, even if they haven’t lost weight? This is sarcopenia—the gradual loss of muscle mass and strength that comes with aging. This same process happens to the muscles in your throat, playing a key role in OSA development.
Neurological changes with age
Muscle weakness isn’t the only problem – aging changes how our brain coordinates breathing during sleep.
Our brain becomes less sensitive to oxygen and carbon dioxide levels as we age.
Bidirectional relationship between aging and OSA
Aging and sleep apnea create a two-way street that can turn into a dangerous cycle.
OSA becomes more common as we age.
Sleep disorders and sarcopenia share a strong connection.
This suggests muscle loss might both cause and result from breathing problems during sleep.
Resources:
- American Academy of Sleep Medicine: https://aasm.org/
- National Institute on Aging: https://www.nia.nih.gov/
- Sleep Foundation: https://www.sleepfoundation.org/
Sleep Apnea and Cognitive Aging: The Brain Connection
Sleep apnea doesn’t just age your body—it can age your brain too. Recent research has uncovered troubling connections between OSA and cognitive decline:
Memory and Executive Function
Studies show that people with untreated sleep apnea experience:
- 40% faster decline in processing speed
- Significant reductions in working memory capacity
- Impaired decision-making abilities even in mild cases
The Alzheimer’s Connection
The link between sleep apnea and Alzheimer’s disease is particularly concerning:
- OSA patients show increased beta-amyloid deposits, a hallmark of Alzheimer’s
- Each 10% drop in oxygen saturation is associated with a 31% increase in beta-amyloid burden
- Poor sleep quality disrupts the brain’s nightly “cleaning” process that removes these harmful proteins
CPAP Treatment: Brain Protection?
The good news: CPAP therapy shows promise for brain health:
- Early intervention appears more effective for preserving cognitive function
- One year of consistent CPAP use preserved white matter integrity in a 2022 study
- Cognitive function improves in as little as 3 months of treatment in some patients
Related post: How to Keep Your Brain Sharp After 40?
Treatment Options That May Slow Aging

Image Source: Health
Sleep apnea treatment does more than just improve sleep quality—it might slow down biological aging. Research shows several treatments could potentially reverse the faster aging linked to OSA, giving hope to people worried about their long-term health.
CPAP therapy and vascular health
Using CPAP for more than 4 hours each night provides major heart health benefits.
Oral appliances and airway support
Oral appliances are a great alternative for patients who can’t use CPAP.
Lifestyle changes and weight management
Weight management is a vital part of OSA treatment.
Can treatment reverse biological aging?
The most exciting finding suggests that effective OSA treatment might reverse faster biological aging.
Recent studies provide encouraging data on how quickly treatment can reverse accelerated aging markers: A landmark University of Missouri study demonstrated that consistent CPAP use (≥5 hours nightly) for one year resulted in DNA methylation patterns consistent with a biological age 3.1 years younger than baseline measurements. This suggests that significant portions of OSA-induced aging can be reversed with diligent treatment adherence. Even more encouraging, improvements in sleep quality, cognitive function, and energy levels typically begin within 1-2 weeks of consistent treatment. Research shows an undeniable link between sleep apnea and faster biological aging. The blood vessel system shows clear signs of early aging in people with sleep apnea. Notwithstanding that, several treatment options work well. Sleep apnea does more than just ruin your sleep quality – it changes how your body ages at its core. Looking at multiple biological markers and long-term studies, undiagnosed and untreated sleep apnea poses a major public health risk that needs more attention. Many cases go unnoticed, but awareness grows as science uncovers more links between poor sleep and faster aging. Resources: While there’s no definitive average age of death for sleep apnea patients, studies show that untreated severe obstructive sleep apnea can significantly increase mortality risk, especially in middle-aged adults. However, effective treatment can potentially add years to life expectancy. Severe sleep apnea can lead to serious cardiovascular issues including increased risk of coronary artery disease, heart attack, heart failure, and stroke. It also raises the likelihood of developing arrhythmias and can negatively impact blood pressure regulation. Yes, aging can contribute to sleep apnea development. Age-related changes such as decreased muscle tone in the upper airway, alterations in sleep architecture, and reduced sensitivity to oxygen and carbon dioxide levels can all increase the risk of developing sleep apnea in older adults. CPAP therapy is highly effective when used consistently. Regular use of CPAP for at least 4 hours nightly can significantly reduce cardiovascular risks, improve blood pressure, and even potentially slow down biological aging processes associated with sleep apnea. Yes, there are alternatives to CPAP therapy. Oral appliances like mandibular advancement devices can be effective, especially for mild to moderate cases. Additionally, lifestyle changes such as weight loss, regular exercise, and avoiding sleeping on your back can help manage sleep apnea symptoms.Reversal Timeline: What Research Shows
Biomarker Improvement Timeline Percentage Improvement Oxidative Stress 3-6 months of CPAP 40-60% reduction in oxidative markers Endothelial Function 1-3 months of CPAP 30% improvement in flow-mediated dilation Telomere Attrition 12+ months of CPAP 20-30% slowing of telomere shortening rate DNA Methylation Age 12+ months of CPAP 2-3 years reduction in epigenetic age Pulse Wave Velocity 6 months of CPAP 10-15% reduction in arterial stiffness Conclusion
FAQs
How does sleep apnea affect life expectancy?
What are the long-term health consequences of severe sleep apnea?
Can the natural aging process contribute to sleep apnea development?
How effective is CPAP therapy in treating sleep apnea?
Are there alternatives to CPAP for treating sleep apnea?