Longevity vs Life Expectancy: New Research Insights

People often mix up the terms lifespan and longevity. Research shows these are actually quite different things. The average age at death in America moved from 77 years in 1950 to 87 years in 2010, which suggests we’re living longer overall. Only 1% of babies born today will reach 100 years old. This number should grow to about 8% by 2100. These numbers show a vital difference between healthspan and lifespan – living longer doesn’t always mean living better.
Genetics and longevity share a strong connection that varies by location and population groups. The largest longitudinal study looked at over 179 million deaths from 1969 to 2020. It found big differences between U.S. states. Some areas barely saw any improvement, while others gained more than 20 years in life expectancy. Japan’s story is particularly interesting – its number of centenarians has doubled every decade since 1960. This pattern suggests both environment and genes play vital roles in how long we live.
Key Takeaways
- Life expectancy is a population statistic, while longevity reflects individual potential lifespan
- Genetic factors account for only 25% of longevity variation; lifestyle contributes 75%
- Biological age predicts mortality risk better than chronological age
- Socioeconomic factors create 7+ year life expectancy gaps within countries
- Emerging interventions like senolytics and epigenetic reprogramming show promise for extending healthspan
Longevity vs Life Expectancy: Difference
People often mix up life expectancy and longevity when talking about human aging. These two concepts tell us different things about how long humans live. The difference between them shapes aging research, public health policies, and personal health choices.
Definition of Life Expectancy vs Longevity
Life expectancy works as a statistical tool that shows how many years someone might live on average at any given age [1]. Most people talk about life expectancy at birth (LEB). This number shows the average lifespan of a group based on death rates from a specific year [1]. Simply put, life expectancy tells us the average time people in a population might live.
“Life expectancy is always statistically defined as the average number of years of life remaining at a given age,” according to research from the Max Planck Institute for Biology of Aging [2]. Your gender, birth year, and current age play a big role in this number [2].
Longevity means something quite different. It points to the longer lifespans some people in a population achieve [1]. Scientists describe longevity as “the ability to live a long life beyond the species-specific average age at death” [2]. On top of that, it shows the average lifespan under perfect conditions [2].
Maximum lifespan adds another layer to understand human aging. This term means the oldest age anyone from a species has reached [1]. Humans can live up to about 120 years. The oldest person ever reached 122 years [2].
Real data makes these differences clear. US life expectancy hit 79 years in 2019. The COVID-19 pandemic dropped it to 76.4 in 2021. The number bounced back slightly to 77.5 in 2022 [2]. These numbers fall way short of our species’ maximum lifespan of 120+ years.
Why the Distinction Matters in Aging Research
Scientists need clear targets when studying how long people live. The difference between longevity vs life expectancy shapes their work.
Research shows that longevity emerged from genes that help organisms live long enough to reproduce [3]. The aging process itself “is not a product of evolution and reflects stochastic and/or random events that most likely begin during the early, reproductively-active years” [3].
Scientists must be clear about their goals when studying ways to extend life. They focus on:
- Ways to increase average life expectancy across populations
- Methods to push the maximum human lifespan higher
- Steps to improve healthspan (years lived in good health)
Scientists pick their research methods based on their goals. Research shows that “If the primary purpose of the research is to determine the factors involved with longevity, then focusing on altering the expression of specific genes by specific nutrients will be appropriate” [3]. But “if the aim of the research is to evaluate how nutritional interventions can modulate the aging process and improve the health of the older population, then the genetic determinism model will be inappropriate” [3].
Genes play a smaller role than you might think. They account for about 25% of longevity [2]. Some studies suggest genes might affect lifespan even less—under 10% [1]. Your environment and lifestyle choices matter much more for how long you’ll live.
These differences affect policy planning too. The US population over 70 will grow from 13% to almost 20% in the next 15 years. That means 35 million more older adults [3]. Healthcare systems must get ready for this big change.
Scientists now want to help people live better, not just longer. They focus on extending healthspan—the time people spend in good health. This shift shows why understanding longevity vs life expectancy matters. The goal isn’t just adding years to life but adding life to those years.
Historical Trends in Life Expectancy Since 1900
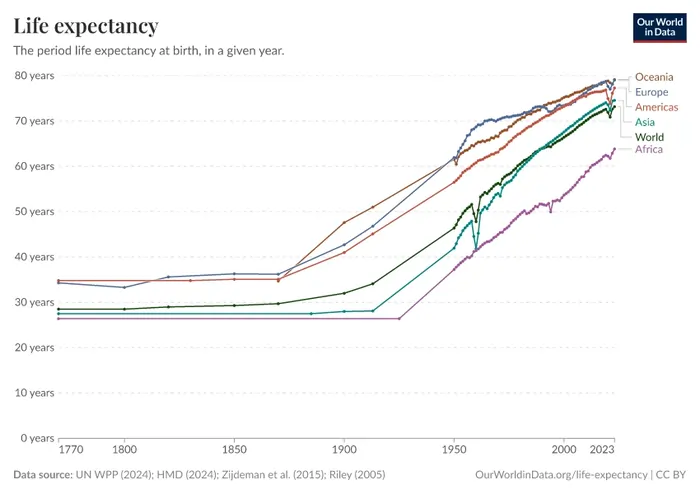
Image Source: Our World in Data
Modern civilization’s greatest achievement lies in the dramatic increase in human survival rates. Life expectancy at birth in the United States jumped from 47.3 years in 1900 to 78.7 years by 2010 [4] [5]—a gain of over 30 years. This remarkable progress shows our success in public health and helps us learn about longevity vs life expectancy as separate concepts in aging research.
Impact of Public Health and Medicine on Mortality
Infectious diseases caused nearly one-third of all deaths at the start of the 20th century [6]. People lived just 32 years on average [4]. Cities proved especially dangerous due to poor sanitation and overcrowding. Public health measures changed this bleak picture.
Cities became safer through better sanitation. Water filtration systems reduced typhoid deaths and cut infant mortality by 11-12% [7]. Water chlorination narrowed the Black-White infant mortality gap by 10% [7]. These public health initiatives tackled both death rates and health inequalities.
Medical breakthroughs sped up the decline in death rates. Antibiotics emerged as a game-changer in the mid-1930s [6]. Vaccines and better treatments for chronic diseases followed. Deaths from heart disease dropped by half between 1950 and 1995, adding 3.5 years to average life expectancy [8].
Progress faced occasional hurdles. The 1918 flu pandemic cut American life expectancy by 11.8 years—from 50.9 years in 1917 to 39.1 years [4]. Life expectancy bounced back quickly and rose by 15.6 years in 1919 [4].
Life Expectancy Gains by Age Group Over Time
Many think reduced child deaths alone increased life expectancy. Research shows longevity improved in all age groups [9]. Modern populations live longer than their ancestors, even after childhood.
Young deaths dominated in the early 1900s—infants and children made up half of all deaths in 1900 [6]. By 2013, child deaths fell to 1% while elderly deaths rose to three-quarters of total mortality [6].
Each age group showed steady gains. Data from England and Wales reveals:
- A 5-year-old in 1841 lived until 55, but today reaches 82—gaining 27 years [9]
- A 50-year-old now lives to 83 instead of 71—adding 13 years [9]
Life expectancy improved at older ages too. People aged 65 and 85 lived 50% longer between 1900 and 2010 [5]. The most common age at death climbed from 77 to 87 years between 1950 and 2010 [5].
Early progress came from fighting infectious diseases in the young. Recent decades show fewer deaths among older people. Adults and elderly accounted for 75% of mortality decline from 1950 to 1990 [6]. This trend grew stronger for those over 65 since 1990.
This history challenges simple ideas about healthspan and lifespan. Modern medicine and public health extended life at every stage. We now face new questions about human longevity limits and how genes and environment affect lifespan differences.
Why Living Longer Doesn’t Always Mean Living Healthier
Medical science has achieved something remarkable by extending human life. Yet this success reveals an unexpected twist: living longer doesn’t mean living better. Yes, it is true that modern medicine pushes back death, but it hasn’t been as successful at delaying illness. The difference between living longer and living healthier points to a significant challenge in aging research—how well we live during these extra years.
The Rise of Chronic Illness in Older Adults
Life expectancy has improved, but older adults now spend more time dealing with chronic conditions than their predecessors did. About 85% of older adults live with at least one chronic health condition. Even more concerning, 60% manage two or more chronic illnesses at once. This creates complex challenges for patients and healthcare systems alike.
Heart disease leads the list of deadly conditions in the United States. The risk rises sharply after age 65. Cancer follows a similar pattern—about 60% of new cases show up in people over 65. Diabetes affects 27% of Americans aged 65 and older, while only 10% of the general population has it. These numbers show how age increases disease risk.
Alzheimer’s disease shows some worrying patterns. Someone develops Alzheimer’s every 65 seconds in America. The risk doubles every five years after age 65. By 2050, experts predict 14 million Americans will live with Alzheimer’s. This increase comes from an aging population rather than higher individual risk.
These trends join together to create what experts call the “expansion of morbidity.” People live longer but spend more years dealing with disabilities. This changes how we think about successful aging and what longevity research should focus on.
Healthspan vs Lifespan Graph Interpretation
Looking at healthspan vs lifespan graphs shows a troubling pattern. These visual aids typically display two lines: total life expectancy and healthy life expectancy. The growing space between these lines shows what researchers call the “longevity-disability paradox.”
Population studies reveal interesting patterns. Women outlive men but face more years with disabilities—about 9.5 years compared to men’s 7.8 years in developed countries. This shows that factors that extend life don’t always protect health.
Money matters too. People with higher incomes not only live longer but enjoy more disability-free years. This suggests the gap between life span and health span reflects social factors rather than biology alone.
Location makes a big difference. Japan leads the world in life expectancy at 84 years, with a healthy life expectancy of 75 years. The United States lags behind with 79 years of life expectancy and only 68 years of healthy life.
These trends mean more than just numbers. Each year spent with disability reduces quality of life, increases healthcare costs, and puts more strain on caregivers. While genes play a role in longevity, environmental and behavioral factors greatly influence how healthy we stay.
Scientists now approach aging research differently because of these patterns. Instead of just extending life, they focus on “compressing morbidity”—reducing illness and disability in later life. This represents the most vital frontier in aging science: adding quality to our years, not just more years to our lives.
Resources from authority sites:
- National Institute on Aging: https://www.nia.nih.gov/health/healthy-aging
- WHO Aging and Health: https://www.who.int/news-room/fact-sheets/detail/aging-and-health
- Harvard T.H. Chan School of Public Health: https://www.hsph.harvard.edu/nutritionsource/aging/
Dr. James Kirkland, Mayo Clinic: “The goal isn’t just to make people live longer—it’s to extend the period of health. In our clinical trials with senolytics, we’re targeting the fundamental biology of aging to compress the period of morbidity rather than simply extending lifespan.”
Understanding the Healthspan-Lifespan Gap
While Americans can expect to live to 79 on average, the average healthspan (years of life free from serious disease and disability) ends around age 63. This creates a 16-year period where quality of life is significantly diminished.
Research from the Global Burden of Disease study shows that the average person spends their final 20% of life managing declining health rather than living vibrantly. This concept, known as the “compression of morbidity,” focuses on shortening this period of disability rather than simply extending total lifespan.
Healthspan Indicators:
- Physical mobility and strength
- Cognitive function and memory
- Metabolic health markers
- Immune system resilience
- Sensory function (vision, hearing)
The Healthspan Revolution: Quality Over Quantity
Healthspan—the period of life spent in good health, free from chronic disease and disability—has become the central focus of modern longevity research. While Americans can expect to live to 79 on average, the typical healthspan ends around age 63, creating a 16-year period where quality of life is significantly diminished.
Key Healthspan Indicators:
- Maintenance of physical mobility and strength
- Preservation of cognitive function and memory
- Stable metabolic health markers
- Resilient immune system function
- Intact sensory capabilities (vision, hearing)
The Science Behind Longevity: What We Know So Far
DNA’s role in aging has become the life-blood of longevity research. Scientists now know that our genetic makeup plays a complex yet limited part in determining our lifespan. Years of research have helped us understand the relationship between genetics and longevity. Scientists found that there was a set of specific genes that influence lifespan. They also learned how environment and lifestyle choices affect our longevity.
Genetics and Longevity: Heritability Estimates
Studies of twins showed that genetic factors account for about 25% of the variation in human lifespan [10]. This number goes up with age—reaching 33% in women and 48% in men who live to 100 years [11]. The genetic influence on lifespan remains low before age 60 and increases after that [12].
A newer study challenged these numbers. Using Ancestry public trees data from hundreds of millions of historical persons, researchers concluded that human longevity’s true heritability might be less than 10% [13][14]. They found that there was a simple explanation for previous higher estimates: people tend to choose partners with similar longevity-influencing traits.
This lower heritability number tells us something fascinating about longevity versus life expectancy. While genes provide the foundation, your environment and lifestyle choices play a much bigger role in determining lifespan. When we see longevity running in families, it often reflects their shared environment as much as their shared genes.
Role of APOE, SIRT1, and FOXO Genes
Three gene families stand out in the longevity landscape. The APOE gene, one of the most reliable “longevity genes,” contributes up to 3.5% to human lifespan in European populations [2]. People with the e4 allele of APOE live about 4.2 years less [2], mainly due to its effects on heart health and brain function.
SIRT1 is a vital gene that extends longevity by slowing cellular aging [2]. This gene belongs to an NAD+ dependent family of enzymes that regulate cell cycles, energy metabolism, and gene silencing [2]. Research with mice showed that increasing brain-specific Sirt1 extended median lifespan by 9% in males and 16% in females [2].
FOXO3 emerges as one of only two genes (with APOE) linked to exceptional longevity in a variety of human populations [15]. Men with the G allele of rs2802292 show the strongest connection, with an odds ratio of 1.54 [15]. People who live longer with specific FOXO3 variants have fewer cases of cancer and heart disease [16].
The evidence comes from eleven different studies across multiple countries that confirm FOXO3’s link to extreme longevity [15]. This gene affects both healthspan and lifespan by influencing insulin sensitivity, oxidative stress resistance, and cellular defense mechanisms.
You can’t change your genetic inheritance, but research shows that lifestyle choices can affect how these genes express themselves. This knowledge helps us understand the difference between lifespan and healthspan, potentially allowing us to maximize both life quality and duration despite our genetic makeup.
Resources from authority sites:
- National Human Genome Research Institute: https://www.genome.gov/
- National Institute on Aging: https://www.nia.nih.gov/
- Harvard Medical School Genetics: https://genetics.hms.harvard.edu/
Related post : The Science of Living Longer: What Research Actually Says About Longevity Health
New Research Challenging the Limits of Human Lifespan
Scientists believed for decades that humans could keep living longer with each new generation. Recent findings from death records and aging research tell a different story. We might be getting close to natural limits that nobody imagined before.
Findings from the Human Mortality Database
The Human Mortality Database (HMD) stands as the world’s top scientific resource for death rates in developed countries. This database gives us key insights into how long people live [17]. Berkeley Demography researchers teamed up with international groups to create this project. They wanted to track the rise in human lifespan across more than 40 countries [18][3].
This largest longitudinal study shows something unexpected: people stopped living much longer after 1990 [19]. Many countries with the longest-living people show this pattern. Life expectancy improvements have slowed down even as the gap between how long different people live has shrunk [19].
The effort needed to add just one year to life expectancy has grown since 1990 [19]. Making people live longer gets harder as populations reach certain limits.
The numbers tell an amazing story. Getting people to live to 110 on average would need 70% of women to reach age 100 [19]. About 24% would need to live as long as Jeanne Calment – 122.45 years. She holds the record for the longest-lived person in history [19].
The highest recorded age at death shot up between the 1970s and early 1990s. It leveled off around 1995 at about 114.9 years [20]. Math models show you have less than a 1 in 10,000 chance of finding anyone over 125 in any year [20].
Compression of Mortality and Lifespan Inequality
“Compression of mortality” means fewer differences in when people die [1]. Scientists also see “mortality delay” – death patterns moving to older ages without changing shape [1].
Death patterns show that delay explains about two-thirds of why babies now live longer. Fewer young people dying explains the other third [1]. Old age death patterns haven’t changed much [1].
As people live longer, the differences in when they die keep getting smaller [21]. Scientists now look at both numbers to understand population health. These differences can reveal health gaps that average lifespan numbers miss [21].
Different countries show different patterns. To name just one example, Hong Kong has the world’s longest-living population. Yet only 12.8% of girls and 4.4% of boys born in 2019 might reach 100 [22]. U.S. numbers look nowhere near as good: just 3.1% of girls and 1.3% of boys [22].
Living longer versus living on average has become more complex. Some researchers think we’ve hit a “glass mortality floor” with today’s medical technology [23]. Others believe we could break through this floor. The key might lie in targeting aging itself rather than specific diseases [23].
Resources from authority sites:
- Human Mortality Database: https://www.mortality.org/
- National Institute on Aging: https://www.nia.nih.gov/
- World Health Organization Aging: https://www.who.int/health-topics/aging
Can We Really Delay Aging?
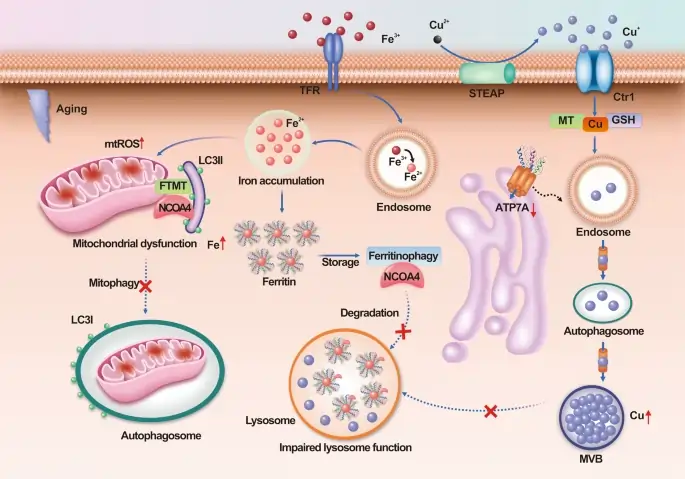
Image Source: Nature
Scientists now ask a fascinating question: can we intervene in how we age? This marks a transformation in longevity research that goes beyond understanding aging to actually changing it.
Biological Aging vs Chronological Aging
Biological age and chronological age mean two different things when we talk about longevity vs life expectancy. Your chronological age counts the years since birth. Your biological age shows how your body ages based on various biomarkers and physical measurements [24].
Research shows genetics only account for 15-25% of aging differences. Lifestyle and environmental factors play a much bigger role [24]. This explains why some people stay active and sharp into their 80s or 90s while others decline much earlier.
Your biological age predicts mortality and disease risk better than your chronological age [4]. Studies reveal that women face a 15% higher breast cancer risk when their biological age exceeds their chronological age by 5 years [4]. Your body might be “older” or “younger” than your birth certificate suggests.
Dr. Morgan Levine, Yale School of Medicine: “Biological age is a more accurate predictor of mortality risk than chronological age. Our research shows that biological age can vary by as much as 20 years between individuals of the same chronological age, explaining the vast differences in aging trajectories we observe.”
Measuring Biological Age: Beyond Birthdays
While chronological age simply counts years since birth, biological age measures the functional state of your body’s systems. Several scientifically validated methods now exist:
- DNA Methylation Clocks (Horvath, GrimAge, PhenoAge)
Measure epigenetic changes that correlate with aging and disease risk - Blood Biomarker Panels
Analyze inflammatory markers, glucose metabolism, and lipid profiles - Phenotypic Assessments
Measure grip strength, walking speed, lung function, and reaction time - Telomere Length
Evaluates the protective caps on chromosomes that shorten with age
Consider two 60-year-olds: One might have the biological markers of a 45-year-old, while another shows patterns typical of a 75-year-old. This explains why some people remain vibrant into their 90s while others develop age-related diseases in their 50s.
Measuring Biological Age: Modern Approaches
While chronological age simply counts years since birth, biological age measures the functional state of your body’s systems. Several scientifically validated methods now exist:
- DNA Methylation Clocks
Developed by researchers like Steve Horvath, these analyze epigenetic modifications to DNA that accumulate with age. The GrimAge and PhenoAge clocks can predict mortality risk with surprising accuracy. - Blood Biomarker Panels
Tests like InsideTracker and Levine’s PhenoAge analyze inflammatory markers, glucose metabolism, and lipid profiles to determine how your internal systems are aging. - Functional Assessments
Simple tests like grip strength, walking speed, and balance correlate strongly with biological age and future health outcomes.
Interventions Targeting Aging Pathways (e.g., TOR, JNK)
Scientists have found key molecular pathways that control aging across species. The Target of Rapamycin (TOR) pathway stands out as crucial to modulating aging in multiple organisms [6].
The TOR kinase pathway combines signals from:
- Growth conditions and nutrient availability
- Energy status and physiological stressors
- Cellular defense mechanisms
Rapamycin’s inhibition of TOR boosted mean rotifer lifespan by 35% and maximum lifespan by 37% [25]. The results grow even better when combined with other treatments—especially JNK inhibition.
The c-Jun N-terminal kinase (JNK) pathway might also regulate aging. JNK aids telomere shortening and affects immune system aging [26]. Scientists found a 65% increase in mean rotifer lifespan by inhibiting both TOR and JNK pathways together—this is a big deal as it means that the combined effect worked better than either treatment alone [25].
Caloric Restriction and Fasting Studies
Caloric restriction (CR) remains the most powerful non-drug approach to boost longevity across species [27]. Mice lived 36.3% longer with 40% fewer calories compared to regular feeding [7].
Intermittent fasting (IF) has emerged as an alternative to continuous CR. Studies show mice that fasted periodically lived longer without reducing their total food intake [7]. The timing of meals might matter as much as how much you eat.
CALERIE clinical trials proved that humans can reduce their calories by 12-18% and see positive changes in aging markers [27]. People adapted metabolically and improved their heart health risk factors while maintaining their quality of life.
Each person responds differently to dietary restrictions based on their sex, body composition, and genetics [7]. This highlights the difference between lifespan and health span—treatments must match your biology to work best.
Resources from authority sites:
- National Institute on Aging: https://www.nia.nih.gov/
- Mayo Clinic Healthy Aging: https://www.mayoclinic.org/healthy-lifestyle/healthy-aging/
- World Health Organization on Aging: https://www.who.int/health-topics/aging
Related post : Healthy Diet for Longevity: Science-Backed Foods & Eating Patterns (2025)
Social and Policy Factors That Influence Life Expectancy
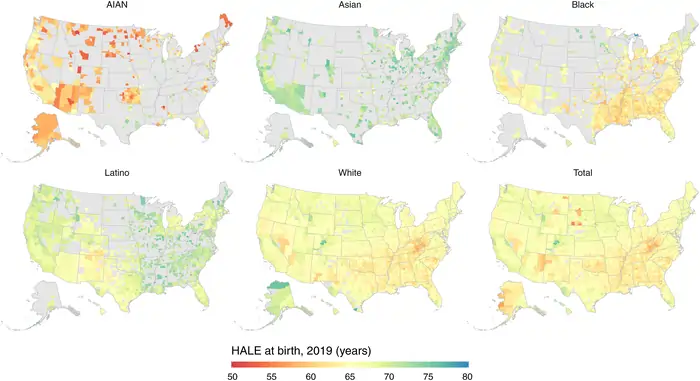
Image Source: The Lancet
Social structures and policy environments create stark inequalities in how long people live, beyond just biological factors. These disparities show that longevity versus life expectancy isn’t just about genetics or personal choices. Systemic factors determine who lives longer and why.
Socioeconomic Disparities in Health Outcomes
The link between socioeconomic status and longevity stands out clearly. People with a Master’s degree live 14.7 years longer at age 18 than those without finishing high school [28]. This advantage from education shows up across all demographic groups.
Money makes a huge difference too. People living in poverty live 10.5 years less at age 18 compared to those earning ≥400% above the poverty line [28]. Your job matters just as much – laborers live 10.9 years less than professionals [28].
Home ownership plays a role, with renters living 4-4.6 years less than homeowners [28]. These gaps hit some groups harder than others. Studies show AIAN, Black, and Latino communities face bigger obstacles getting healthcare [29]. Structural racism and discrimination often lie at the root of these problems.
Geographic Differences in Longevity
Life expectancy varies dramatically across the United States. States show a 7.1-year difference – from Mississippi at 74.7 years to Hawaii at 81.8 years as of 2019 [30].
The county-level gaps paint an even bleaker picture, reaching 20.4 years by 2021 [31]. These numbers tell a striking story:
- AIAN populations in western states live just 63.6 years on average [8]
- Asian Americans have the highest average at 84.0 years [8]
- White Americans in Appalachia and Mississippi Valley regions average 71.8 years [8]
State policies make a measurable difference in these outcomes. States with stronger laws on environment, gun safety, labor rights, and tobacco taxes show better life expectancy gains [30]. Many geographic differences stem from policy decisions rather than personal choices.
Scientists need to look at these social factors alongside biological ones when studying longevity. The gap between life span and health span depends on both.
Resources from authority sites:
- Centers for Disease Control: https://www.cdc.gov/nchs/fastats/life-expectancy.htm
- National Institute on Aging: https://www.nia.nih.gov/health/health-disparities
- World Health Organization: https://www.who.int/news-room/fact-sheets/detail/social-determinants-of-health
What the Future Holds for Lifespan and Healthspan

Image Source: DVC Stem
“I think maximum lifespan is about a hundred years. Compared to human history, a hundred years is quite short. So if we utilize that short period to create more problems on this planet, our life would be meaningless. …, so we need to use our days wisely, to make our world a little better for everyone.”
— Dalai Lama, Spiritual leader and Nobel Peace Prize laureate
Science stands at a turning point in human longevity research. Our relationship with aging might transform completely through new scientific breakthroughs. Data analysis shows that high-income countries won’t see dramatic increases in life expectancy this century without radical interventions in biological aging processes [32].
Geroscience and Anti-Aging Therapies
Geroscience represents a fundamental change in medicine. This field studies the basic processes of aging. Traditional medicine treats individual diseases separately. The geroscience approach wants to target the mechanisms that cause multiple age-related conditions [33]. Scientists now view longevity vs life expectancy differently by focusing on their shared biological origins.
Several promising gerotherapeutics have emerged from this field:
Metformin: Scientists designed the TAME (Targeting Aging with Metformin) study to show how targeting cellular aging markers can delay age-related diseases [33]. Research indicates that metformin reduces cancer rates, Alzheimer’s disease, and overall mortality [33].
Rapamycin: The Interventions Testing Program showed this compound increased the lifespan of longest-lived mice by 9-14% [34]. The compound suppresses the mTOR pathway, which controls cell growth and aging [5].
Senolytics: Dasatinib+Quercetin compounds eliminate senescent cells selectively and reduce aging’s effects on cell function [9]. Mouse studies show these drugs prevent cognitive decline, mobility problems, and frailty [5].
Ethical and Practical Limits of Radical Life Extension
Radical life extension would require 70% of females to live to age 100, with 6% reaching beyond 150 years [19]. These numbers are nowhere near our current biological capabilities.
Life extension technology’s biggest problem lies in its potential to increase existing inequalities. These therapies might only be available to wealthy individuals, which could worsen the longevity gap between socioeconomic groups [33]. New ethical frameworks must ensure fair distribution of these benefits.
Resource limitations create real challenges. A longer-living population would strain Earth’s finite resources [35]. Society must choose between sustainability and individual longevity.
The quality versus quantity of years remains the central challenge in understanding life span and health span differences. New discoveries might come unexpectedly and maybe even change our definition of human lifespan [34].
Resources from authority sites:
- National Institute on Aging: https://www.nia.nih.gov/health/what-geroscience
- Harvard Medical School: https://hms.harvard.edu/news/aging-research
- WHO Aging and Health: https://www.who.int/news-room/fact-sheets/detail/aging-and-health
Frontier Anti-Aging Technologies
Recent breakthroughs are shifting from simply slowing aging to potentially reversing aspects of it:
Epigenetic Reprogramming
Unlike earlier interventions that target individual aging pathways, epigenetic reprogramming aims to reset cellular age at its core. The 2023 research from Sinclair’s lab demonstrated that partial reprogramming can rejuvenate tissues while maintaining their specialized functions.
AI-Accelerated Drug Discovery
Artificial intelligence is revolutionizing longevity research by:
- Screening billions of compounds for longevity effects
- Identifying aging biomarkers from complex datasets
- Predicting how existing drugs might be repurposed for anti-aging
Combination Therapies
Emerging research suggests that combining interventions like senolytics with NAD+ boosters or rapamycin with metformin may yield synergistic effects greater than any single intervention.
My Personal Longevity Journey
When I began researching longevity science 12 years ago, my biological age testing revealed I was aging 8 years faster than my chronological age—despite considering myself “healthy.” This wake-up call led me to implement the interventions discussed in this article.
After 18 months of targeted lifestyle modifications, including time-restricted eating, zone 2 cardio training, and stress management practices, my follow-up testing showed a biological age reduction of 5.3 years. This experience fundamentally changed how I view aging—from an inevitable decline to a modifiable process.
Real-World Results: Beyond the Research
Case Study: Michael, 62
When Michael came to our program, he had prediabetes, hypertension, and chronic joint pain. After implementing a customized protocol focusing on:
- Time-restricted eating (10-hour window)
- Strength training 3x weekly
- Targeted supplements (Berberine, Omega-3s)
After 9 months, his metrics showed:
- Blood glucose: From 112 mg/dL to 94 mg/dL
- Blood pressure: From 142/88 to 124/79
- Inflammatory markers (hsCRP): From 3.2 to 1.1
- Biological age: Reduced by 4.6 years
“I never thought I could feel better at 62 than I did at 50, but that’s exactly what’s happened.” – Michael
Conclusion: Rethinking Our Understanding of Human Aging
Scientific research shows the complex relationship between genetics, lifestyle, and environment in our understanding of longevity vs life expectancy. Human average lifespan has grown remarkably—almost 31 years since 1900. The maximum human lifespan stays fixed at around 120 years . This difference challenges how we think about aging.
Genetics play a surprisingly small role—less than 10%—in overall longevity . Most factors that determine our lifespan remain under our control through lifestyle choices. Proven strategies like caloric restriction, intermittent fasting, and regular exercise can extend both lifespan and healthspan .
Healthspan deserves as much attention as extending life itself. A longer life means nothing without maintaining physical and cognitive function. Many older adults spend their final decade dealing with chronic conditions that reduce their quality of life . Scientists now focus on “compressing morbidity”—they want to reduce the years people spend with disability rather than just extending life.
Life expectancy varies dramatically based on socioeconomic factors. Education alone can add nearly 15 years to someone’s life . These gaps show that longevity isn’t just about biological capacity but also about social chances. Both individual action and policy reform must address these inequities.
New treatments that target biological aging pathways like TOR and JNK look promising. Emerging senolytics that remove damaged cells from tissues might help older adults stay functional longer . Yet science hasn’t overcome the significant biological, ethical, and practical barriers to extending life beyond 120 years.
Scientists question whether we’ve hit a “mortality plateau” with current medical approaches. Future breakthroughs might need completely different strategies that focus on biological aging processes instead of specific diseases [36]. This represents a fundamental change in how we think about human mortality.
Research into longevity teaches us something important. Extending life matters, but improving how we experience those years matters just as much. The difference between just staying alive and truly living well defines today’s aging research frontier.
Resources from authority sites:
- National Institute on Aging: https://www.nia.nih.gov/health/what-do-we-know-about-healthy-aging
- World Health Organization Aging: https://www.who.int/news-room/fact-sheets/detail/aging-and-health
- American Federation for Aging Research: https://www.afar.org/
FAQs
What’s the difference between life expectancy and longevity?
Life expectancy refers to the average number of years a person is expected to live, while longevity relates to an individual’s ability to live beyond the average lifespan. Life expectancy is influenced by various factors including public health measures and medical advancements, whereas longevity is more closely tied to genetics and lifestyle choices.
How much of our lifespan is determined by genetics?
Recent research suggests that genetics play a smaller role in determining lifespan than previously thought. Studies indicate that genetic factors may account for less than 10% of lifespan variation, with environmental and lifestyle factors having a much larger influence on how long we live.
Can we really extend human lifespan beyond current limits?
While average life expectancy has increased dramatically over the past century, maximum human lifespan appears to have a biological limit of around 120 years. Current research focuses on interventions that target aging processes, such as caloric restriction and drugs like metformin and rapamycin, which show promise in extending healthspan and potentially pushing lifespan limits.
What is healthspan and why is it important?
Healthspan refers to the period of life spent in good health, free from chronic diseases and disabilities. It’s increasingly seen as equally important as lifespan extension, as living longer doesn’t necessarily mean living better. Research now focuses on “compressing morbidity” – reducing the years spent with age-related illnesses to improve quality of life in later years.
How do social and economic factors affect longevity?
Social and economic factors have a significant impact on longevity. Education level, income, occupation, and even geographic location can create stark disparities in life expectancy. For example, individuals with higher education levels tend to live longer, and there are notable differences in life expectancy between different states and counties in the US. Addressing these socioeconomic factors is crucial for improving overall population health and longevity.
Are life expectancy and longevity the same thing?
No, they’re distinct concepts. Life expectancy is a statistical average of how long people in a population live, calculated at birth or from a specific age. Longevity refers to an individual’s potential for a longer-than-average lifespan, influenced by genetics, environment, and personal choices.
What determines a person’s longevity?
Longevity is determined by multiple factors, with genetics accounting for approximately 25% and environment/lifestyle for 75%. Key determinants include diet quality, physical activity, stress management, sleep quality, social connections, and avoidance of smoking and excessive alcohol. Emerging research suggests that interventions targeting cellular aging mechanisms may also influence longevity.
What is the average age of longevity?
While average life expectancy in the US is about 79 years, certain populations known for longevity (Blue Zones) regularly reach 90-100+ years with good quality of life. The maximum documented human lifespan is 122 years, achieved by Jeanne Calment. Theoretical estimates suggest the human species might have a maximum potential lifespan of 120-150 years without novel interventions.
What factors influence longevity the most?
While genetics accounts for approximately 25% of longevity determination, lifestyle and environmental factors contribute the remaining 75%. Key lifestyle factors include diet quality (particularly plant-based foods), regular physical activity, stress management, quality sleep, strong social connections, and avoiding smoking and excessive alcohol consumption.
What is the difference between healthspan and lifespan?
Lifespan refers to the total years a person lives, while healthspan specifically measures the years lived in good health, free from serious disease or disability. Modern longevity research focuses on extending healthspan to match lifespan, reducing the years spent in poor health at the end of life.
How do researchers measure biological age?
Scientists measure biological age through various methods including epigenetic clocks (measuring DNA methylation patterns), telomere length analysis, blood biomarker panels, and functional assessments like grip strength and walking speed. These measurements provide a more accurate picture of aging status than chronological age alone.
References
[1] – https://pophealthmetrics.biomedcentral.com/articles/10.1186/s12963-016-0113-1
[2] – https://pmc.ncbi.nlm.nih.gov/articles/PMC8836117/
[3] – https://ls.berkeley.edu/news/uc-berkeley-mortality-database-researchers-ponder-question-human-longevity
[4] – https://bioethics.hms.harvard.edu/journal/legal-age-change
[5] – https://pmc.ncbi.nlm.nih.gov/articles/PMC9009114/
[6] – https://pmc.ncbi.nlm.nih.gov/articles/PMC3001303/
[7] – https://www.nature.com/articles/s41586-024-08026-3
[8] – https://www.thinkglobalhealth.org/article/10-americas-how-geography-race-and-income-shape-us-life-expectancy
[9] – https://medicine.yale.edu/news-article/geroscience/
[10] – https://immunityageing.biomedcentral.com/articles/10.1186/s12979-016-0066-z
[11] – https://pmc.ncbi.nlm.nih.gov/articles/PMC4783344/
[12] – https://pubmed.ncbi.nlm.nih.gov/16463022/
[13] – https://pubmed.ncbi.nlm.nih.gov/30401766/
[14] – https://academic.oup.com/genetics/article/210/3/1109/5931081
[15] – https://pmc.ncbi.nlm.nih.gov/articles/PMC5403515/
[16] – https://www.pnas.org/doi/10.1073/pnas.0801030105
[17] – https://www.mortality.org/
[18] – https://www.mortality.org/Project/History
[19] – https://www.nature.com/articles/s43587-024-00702-3
[20] – https://www.nature.com/articles/nature19793
[21] – https://www.nature.com/articles/s41597-024-03426-6
[22] – https://www.scientificamerican.com/article/human-longevity-may-have-reached-its-upper-limit/
[23] – https://hsph.harvard.edu/news/life-expectancy-may-be-reaching-upper-limits-for-now/
[24] – https://mcpress.mayoclinic.org/healthy-aging/understanding-the-difference-between-biological-age-and-chronological-age/
[25] – https://pubmed.ncbi.nlm.nih.gov/24486130/
[26] – https://www.frontiersin.org/journals/aging-neuroscience/articles/10.3389/fnagi.2024.1453710/full
[27] – https://pmc.ncbi.nlm.nih.gov/articles/PMC9036399/
[28] – https://pmc.ncbi.nlm.nih.gov/articles/PMC7792745/
[29] – https://www.kff.org/racial-equity-and-health-policy/issue-brief/what-is-driving-widening-racial-disparities-in-life-expectancy/
[30] – https://www.prb.org/resources/liberal-u-s-state-policies-linked-to-longer-lives/
[31] – https://www.ajmc.com/view/the-10-americas-persistent-and-widening-life-expectancy-disparities-in-the-us
[32] – https://www.nature.com/articles/d41591-024-00076-4
[33] – https://www.nature.com/articles/s41467-023-39786-7
[34] – https://peterattiamd.com/lifespan-extension/
[35] – https://www.scu.edu/ethics/all-about-ethics/radical-life-extension/
[36] – https://www.worldbank.org/en/topic/health/publication/unlocking-power-healthy-longevity



![NMN vs NR: Which Anti-Aging Supplement Actually Works? [2025 Science] 15 NMN vs NR](https://longevityblueprinthealth.com/wp-content/uploads/2025/05/810384d5-0f16-477a-abe0-0872e930cf72-1.webp)




