How to Stop Insulin Resistance from Aging You Faster: A Doctor’s Guide

Did you know that 40% of U.S. adults have insulin resistance? That’s nearly half of America silently battling a condition that speeds up aging and increases the risk of multiple age-related diseases.
Insulin resistance goes beyond diabetes now. Research shows it plays a crucial role in developing cardiovascular disease, fatty liver disease, and even neurodegenerative conditions. The risk of developing insulin resistance grows as we age – even with a healthy lifestyle.
But there’s hope. Simple lifestyle changes can improve insulin sensitivity by a lot. A 10% reduction in weight can revolutionize your metabolic health. Regular physical activity helps protect against aging’s effects on your insulin response.
My experience as a doctor has helped many patients reverse their insulin resistance and slow down their aging process. This piece will show you effective strategies that work. You’ll learn about risk factors and get a proven 30-day reset plan.
Let’s discover how you can take control of your metabolic health and age better, starting today.
The Aging-Insulin Connection: Understanding the Science
The way aging and insulin interact sits at the heart of many diseases that come with age. Our bodies change how they respond to this vital hormone as we get older. These changes can speed up or slow down the aging process.
How insulin affects cellular aging processes
Insulin shapes almost every part of human physiology and does much more than just control blood sugar [1]. Scientists have found a strong link between insulin signaling and how long we live. People who age well and live longer usually have bodies that respond better to insulin [1].
Inside our cells, insulin does more than regulate metabolism. It helps brain cells adapt, survive, and function properly [1]. Research shows that insulin protects nerve cells and makes memory and thinking better when it reaches the brain directly [1].
All the same, having high insulin levels over time creates an unexpected problem. Too much insulin makes the body store more fat, produce too many proteins, and build up proteins that don’t work [2]. This stresses cells in several ways:
- Cell cleanup systems stop working properly
- Energy-producing parts of cells break down and create harmful substances
- Cells age faster and stop working
- Blood vessels become less healthy
These cellular changes make us age faster and become more likely to develop conditions like Alzheimer’s disease [3].
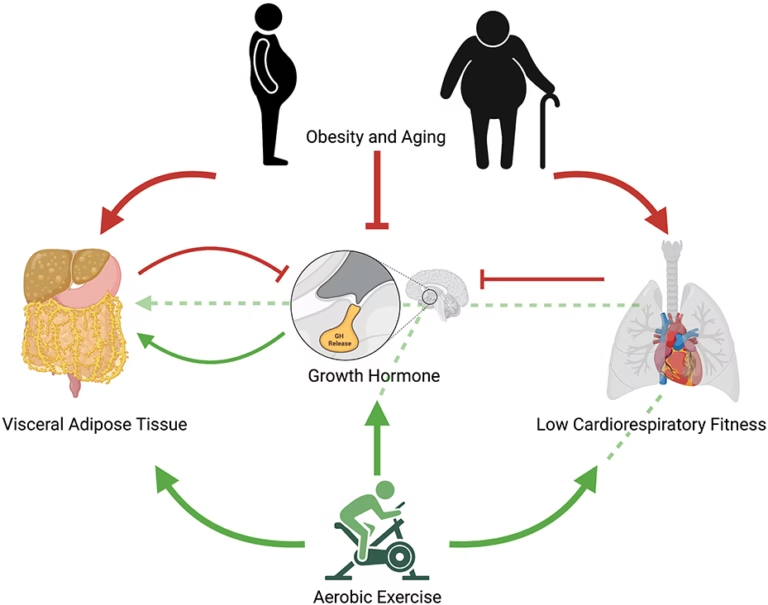
The vicious cycle of age-related insulin resistance
Our ability to handle sugar gets worse as we age. Studies show that problems with blood sugar and type 2 diabetes become much more common in older people – affecting 75.6% of those who are 75 or older [3]. This creates a harmful loop.
Age brings several changes that make insulin less effective:
- More fat builds up around organs and causes inflammation
- Cell powerhouses don’t make energy as well
- Fat accumulates inside muscle cells
- Cells experience more stress
- Muscles become smaller and weaker
Scientists have found a specific enzyme (MT1-MMP) that increases with age and directly damages insulin receptors, which makes insulin substantially less effective [4]. Older mice have high levels of this enzyme, just like young obese mice [4].
This cycle works like this: aging makes insulin less effective, so the body produces more insulin to compensate. Higher insulin levels then stress cells more, which speeds up aging [1].
Research on people who live past 100 and their children shows they respond to insulin better than typical older adults [5]. This suggests that keeping insulin working properly might help us live longer and stay healthier as we age.
Measuring Your Insulin Resistance Risk
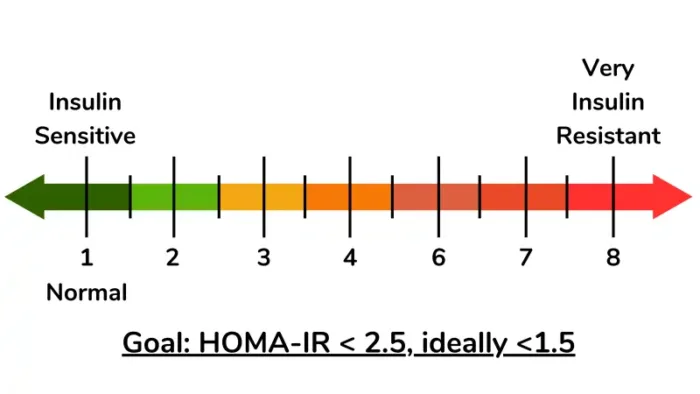
Image Source: Nourished by Science
Insulin resistance develops quietly in your body, often without obvious symptoms until it has advanced substantially. Early detection gives you the best chance to reverse this condition before it speeds up aging and leads to serious health issues.
Self-assessment tools and questions
Your risk factors help determine if you need additional testing. Here are key risk indicators to think over:
- Physical warning signs: Dark, velvety patches of skin around your neck or armpits (acanthosis nigricans) can signal insulin resistance [6]
- Body composition: Your waist size above 88 cm (35 inches) for women or 102 cm (40 inches) for men points to increased risk [7]
- Medical history: Previous gestational diabetes, polycystic ovary syndrome (PCOS), or pre-eclampsia all lift your risk [6]
- Family patterns: Parents or siblings with type 2 diabetes increase your likelihood [8]
- Lifestyle factors: Lack of exercise, poor diet, smoking, excessive alcohol, or night work all add to your risk [6]
Home-testing options now give you more ways to check your health. These kits measure fasting glucose levels and while not as accurate as clinical tests, they help you learn about your metabolic health.
When to seek medical testing
The American Diabetes Association recommends screening at age 45 for most adults [8]. You should get tested earlier if you:
- Have overweight or obesity with other risk factors
- Come from higher-risk ethnic groups (African American, Latino, Native American, Asian American, or Pacific Islander) [9]
- Have high blood pressure (140/90 mm Hg or above) [8]
- Show signs of prediabetes
- Had a baby weighing more than 9 pounds [8]
Children and teens aged 10-18 should get screened if they have overweight plus two or more diabetes risk factors [8].
Understanding your lab results
Doctors use several tests to check for insulin resistance. Each test serves a specific purpose:
Hemoglobin A1C Test: This shows your average blood glucose over about three months.
- Normal: Below 5.7%
- Prediabetes: 5.7% to 6.4%
- Diabetes: 6.5% or higher [8]
Fasting Plasma Glucose (FPG): This test requires fasting for at least 8 hours.
- Normal: Under 100 mg/dL
- Prediabetes: 100 to 125 mg/dL
- Diabetes: 126 mg/dL or higher [8]
Oral Glucose Tolerance Test (OGTT): You drink a sugary solution after fasting, then get blood drawn two hours later.
- Normal: Under 140 mg/dL
- Prediabetes: 140 to 199 mg/dL
- Diabetes: 200 mg/dL or higher [8]
Fasting Insulin Test: This less common test helps detect early insulin resistance.
- Optimal range: 2.6 to 24.9 mcIU/ml
- Values above 7 might indicate higher metabolic syndrome risk [10]
Your doctor might calculate your HOMA-IR score using a formula that combines fasting glucose and insulin levels. A score above 2.9 could suggest substantial insulin resistance [10].
Resources:
- American Diabetes Association: www.diabetes.org
- National Institute of Diabetes and Digestive and Kidney Diseases: www.niddk.nih.gov
The 30-Day Plan to Reset Insulin Sensitivity
Reversing insulin resistance needs a step-by-step plan that helps your body respond better to insulin. This 30-day plan splits the process into weekly phases. Each phase tackles different parts of how insulin works.
Week 1: Eliminating insulin triggers
Your first task is removing the main foods that cause insulin resistance. Research shows that much of the American population (at least 40%) has insulin resistance [11]. These foods often trigger the condition. This week you should:
- Cut refined carbohydrates and added sugars – These make blood glucose spike fast and keep insulin resistance going [12]
- Eliminate ultra-processed foods – Hidden sugars and unhealthy fats in these foods cause inflammation [13]
- Reduce snacking – Eating too often keeps insulin levels high [14]
The original changes might be tough, but losing even a small amount of weight by limiting calories (about 1,200 daily) can help reverse liver insulin resistance by a lot [15].
Week 2: Introducing insulin-sensitizing foods
The next step focuses on adding foods that help insulin work better. You should eat:
High-fiber options – Fiber makes digestion slower and stops blood sugar spikes. Choose whole grains, fruits, vegetables, beans and legumes [1].
Protein with most meals – Protein slows down how your body processes carbs and keeps you full longer. Good sources include lean meats, fish, eggs, and Greek yogurt [1].
Healthy fats – Olive oil, avocados, and fatty fish have omega-3s that help your body use insulin better [16].
Week 3: Optimizing meal timing and frequency
The timing of your meals affects how insulin works in your body. Studies show that:
Having 2-3 balanced meals earlier in the day helps your body respond to insulin better [17]. You might want to limit your eating to less than 10 hours daily. This helps with weight loss and blood sugar control [18].
Missing breakfast throws off your body’s natural rhythm [18]. Eating most of your food in the morning helps control your weight better [19].
Week 4: Fine-tuning your individual-specific approach
The last week helps you create your own plan based on how your body responds. The American Diabetes Association says there’s no “one-size-fits-all” diet to control insulin resistance [20].
Keep track of your:
- Energy levels
- Sleep quality
- Hunger patterns
- Mood stability
Make changes to portions, timing, and food combinations that suit you best. Unlike short-term diets, this becomes a way of life that lasts. Studies prove that an 8-week simple lifestyle change program can reduce insulin resistance effectively [21].
Resources:
- American Diabetes Association: www.diabetes.org
- National Institute of Diabetes and Digestive and Kidney Diseases: www.niddk.nih.gov
Movement Patterns That Combat Insulin Resistance
Image Source: Ruled Me
Your body’s strategic movement throughout the day protects you against insulin resistance. Research shows that physical activity helps your cells respond better to insulin. These benefits go way beyond what diet changes alone can do.
Daily non-exercise activities that improve insulin function
Science proves that sitting too much hurts your metabolic health [3]. The good news is that simple movements in your daily routine can boost insulin sensitivity without formal exercise.
Non-exercise activity thermogenesis (NEAT) – the energy you use during regular activities like walking, standing, and household chores – is vital for metabolic health [22]. Studies of patients with abdominal obesity show that higher NEAT scores link to lower serum insulin levels, which points to better insulin sensitivity [22].
These science-backed strategies work well:
Post-meal walking: Walk within 2 hours after eating, even if just for 2 minutes. A 15-30 minute walk gives you the best results [3]. This simple habit can lower your after-meal glucose levels.
Strategic standing: Standing up throughout your day lowers after-meal glucose levels by about 9.5% [3]. You could use a standing desk or walk while on phone calls.
Everyday movement: Cleaning, gardening, taking stairs, and parking far from entrances add up to give you metabolic benefits [22].
The minimum effective exercise dose
Movement helps, but structured exercise gives you the best benefits for insulin sensitivity. A single 45-minute session of moderate exercise can improve your insulin sensitivity right away [23].
You should aim for:
- Moderate-intensity aerobic activity: 150-300 minutes weekly (about 30 minutes, 5 days/week) [3]
- Vigorous-intensity aerobic activity: 75-150 minutes weekly [3]
- Resistance training: At least 2 days weekly that works all major muscle groups [3]
Research shows that mixing resistance and aerobic exercise works better than doing just one type [24]. Each type works differently: aerobic exercise helps use glucose while resistance training builds muscle that stores glucose better [24].
High-intensity interval training (HIIT) can save you time. It improves insulin sensitivity even with shorter workouts [25].
Resources:
- American Diabetes Association: www.diabetes.org
- American College of Sports Medicine: www.acsm.org
- National Institute of Diabetes and Digestive and Kidney Diseases: www.niddk.nih.gov
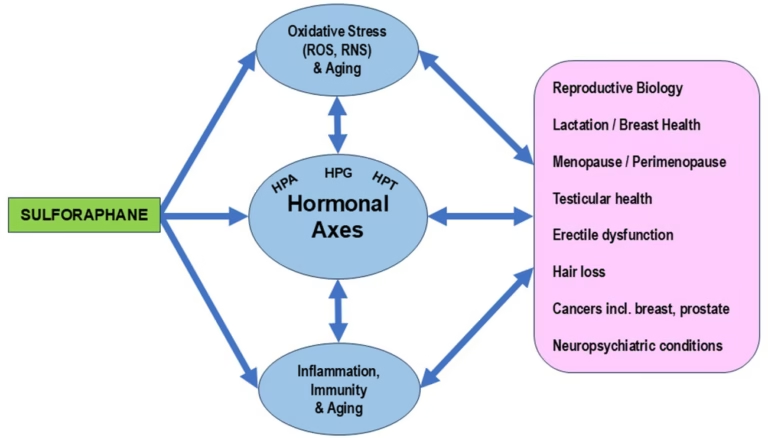
Lifestyle Factors Beyond Diet and Exercise
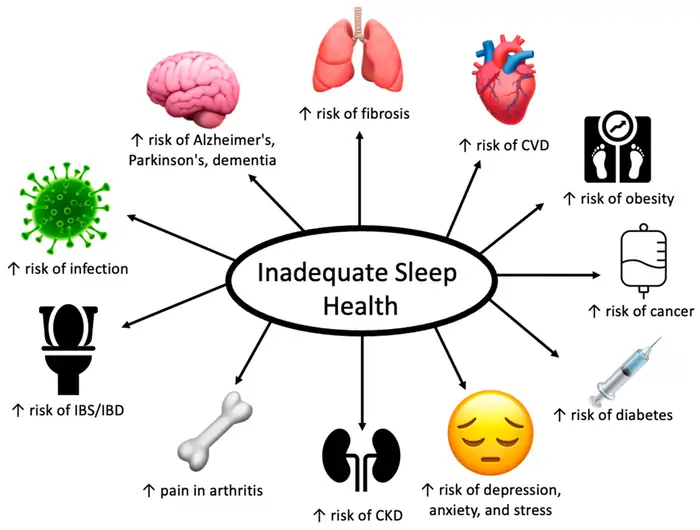
Image Source: MDPI
Diet and physical activity aren’t the only lifestyle factors that affect insulin function. A complete approach to curbing insulin resistance and slowing down aging needs to address several other key elements.
Stress management techniques with proven benefits
Your body responds to chronic stress with hormonal changes. High cortisol levels directly reduce insulin sensitivity [26]. Research shows stress hormones make your liver release glucose, which raises blood sugar even when you haven’t eaten [27].
The good news is that several stress-reduction methods work well:
- Mindfulness meditation: Studies show this practice improves metabolic health and insulin response by lowering cortisol levels [28]
- Regular aerobic exercise: Research found just two workouts per week substantially reduced anxiety levels [2]
- Strategic supplementation: Evidence points to magnesium and vitamin B6 helping lower stress levels [2]
Sleep optimization for hormonal balance
Sleep quality plays a crucial role in insulin sensitivity. Your body can become insulin resistant after just one night of poor sleep [2]. The good news is that making up for lost sleep can reverse these negative effects [27].
To sleep better:
- Keep your sleep and wake times consistent
- Get 7-9 hours of sleep each night [29]
- Stop caffeine intake 6 hours before bed [2]
- Cut down on evening blue light exposure
- Set your bedroom temperature between 60-68°F [2]
Environmental toxins that promote insulin resistance
New research connects environmental pollutants to metabolic problems. Studies have found strong links between insulin resistance and exposure to phthalates, air pollutants, arsenic, and certain pesticides [5].
Extended exposure to air pollution, especially inhalable particulate matter (PM2.5 and PM10), leads to higher insulin resistance markers [30]. On top of that, plastic chemicals, certain pesticides, and heavy metals harm mitochondrial function and create oxidative stress that disrupts insulin signaling [31].
You can protect yourself by:
- Filtering your drinking water, especially from untested wells [32]
- Buying organic produce when possible
- Using fewer plastic food containers
- Getting a home air filtration system
Resources:
- American Diabetes Association: www.diabetes.org
- National Institute of Environmental Health Sciences: www.niehs.nih.gov
- American Academy of Sleep Medicine: www.aasm.org
Supplements and Medications That Help Reverse Insulin Resistance
Lifestyle changes are the foundations of insulin resistance treatment. Strategic supplements and medications can provide extra support. You can improve insulin sensitivity by combining these approaches with proper medical guidance.
Evidence-based supplements for insulin sensitivity
Research shows several supplements can enhance insulin sensitivity. Studies reveal that probiotics help reduce fasting blood glucose and HbA1c levels (0.43% decrease) compared to placebo [33]. Magnesium supplements effectively lower fasting blood glucose but not HbA1c. This benefit becomes more apparent if you have magnesium deficiencies [34].
Here are other supplements backed by science:
- Chromium: Shows very low certainty evidence of lowering HbA1c by 0.54% [34]
- Vitamin C: Associated with improved insulin production and secretion [4]
- Omega-3 fatty acids: Help with breaking down fats and decreasing fat accumulation [29]
- Inositol: Works best for PCOS-related insulin resistance [35]
- Zinc: Supports blood glucose management and improves fasting insulin levels [4]
The right time for medication
Doctors haven’t approved any medications specifically for insulin resistance alone [36]. However, certain diabetes medications can improve insulin sensitivity effectively. Metformin leads the treatment options. It works by reducing hepatic glucose output and helps tissues absorb more glucose [37]. The medication offers modest weight reduction benefits and better lipid profiles [38].
Thiazolidinediones (TZDs) like pioglitazone directly reduce insulin resistance [38]. A multicenter trial showed that pioglitazone lowered stroke and myocardial infarction risk in insulin-resistant patients. The study also found increased risks of weight gain, edema, and fracture [38].
Working with your doctor to create an integrated plan
Your relationship with healthcare providers plays a crucial role in treatment success. Research shows patients respond better to insulin treatment when doctors and nurses encourage them [39].
Clear communication makes a difference. Patients stick to their treatment plans when physicians explain benefits, address concerns, and make decisions together [40]. Research shows poor medication adherence among patients who aren’t happy with their physician interactions [40].
Regular follow-ups help doctors adjust your treatment plans. Patients do better when they have consistent doctors who provide continuous care [41].
Resources:
- American Diabetes Association: www.diabetes.org
- National Institute of Diabetes and Digestive and Kidney Diseases: www.niddk.nih.gov
Conclusion
Good insulin sensitivity is the life-blood of aging gracefully. Research shows that small but consistent changes create the most important improvements to your metabolic health and longevity markers.
Your body naturally rebuilds insulin sensitivity when you follow the 30-day reset plan with dietary changes. Simple post-meal walks and structured exercise sessions increase these benefits further. The quality of your sleep, how you handle stress, and your environment all play crucial roles in transforming your metabolism.
Science proves that people with good insulin sensitivity age better and live longer. Anyone can boost their metabolic health through the right nutrition, movement, and lifestyle changes. The process of reversing insulin resistance needs patience – you should focus on steady progress instead of perfection.
Better insulin sensitivity might seem hard to achieve at first. Breaking it into smaller steps makes lasting change possible. These evidence-based strategies will improve your metabolic health when you start using them today.
Additional Resources:
- National Institute of Health: www.nih.gov/diabetes
- American Diabetes Association: www.diabetes.org
- World Health Organization: www.who.int/diabetes
FAQs
What are some effective ways to quickly improve insulin sensitivity?
Improving insulin sensitivity can be achieved through a combination of lifestyle changes. Focus on losing weight if needed, increasing physical activity, and following a balanced diet low in refined carbohydrates and added sugars. In some cases, your doctor may recommend insulin-sensitizing medications to help manage insulin resistance.
Can vitamin D supplementation help with insulin resistance?
Some research suggests that vitamin D may play a protective role against insulin resistance. Vitamin D is believed to help reduce inflammation, which is associated with an increased risk of insulin resistance. However, it’s important to consult with your healthcare provider before starting any new supplement regimen.
What types of exercise are most beneficial for managing insulin resistance?
A combination of aerobic and resistance training is most effective for improving insulin sensitivity. Aim for at least 150 minutes of moderate-intensity aerobic activity per week, such as brisk walking, cycling, or swimming. Additionally, incorporate strength training exercises at least twice a week to build muscle mass, which can enhance glucose uptake and insulin sensitivity.
Which foods should I include in my diet to reduce insulin resistance?
Focus on consuming foods that are high in fiber, lean protein, and healthy fats. Include whole grains, legumes, fruits, vegetables, fatty fish, nuts, and seeds in your diet. Replace saturated and trans fats with healthier options like olive oil and avocados. Also, opt for low-fat dairy products to get calcium and protein without excess calories.
How does sleep affect insulin sensitivity?
Quality sleep plays a crucial role in maintaining healthy insulin sensitivity. Even one night of poor sleep can temporarily induce insulin resistance in otherwise healthy individuals. Aim for 7-9 hours of sleep per night, maintain a consistent sleep schedule, and create a sleep-friendly environment by keeping your bedroom cool and dark. Improving your sleep habits can significantly benefit your overall metabolic health.
References
[1] – https://www.eatingwell.com/article/8027946/meal-plan-for-insulin-resistance/
[2] – https://www.veri.co/learn/what-causes-insulin-resistance-not-diet?srsltid=AfmBOopQsnU7Vo4lSwVT6gfowEKADBMtGRHUND3y8Rzbwyb-q1FnRpmc
[3] – https://www.veri.co/learn/best-exercises-for-insulin-resistance?srsltid=AfmBOor6EK9nmEoGtyl3GTYwy2NTJIkjaaJe6b4nAAwRQR3ivx9vvvN_
[4] – https://www.rupahealth.com/post/best-supplements-to-help-with-your-insulin-resistance
[5] – https://pmc.ncbi.nlm.nih.gov/articles/PMC3855520/
[6] – https://www.questhealth.com/product/insulin-resistance-test-panel-36509M.html?srsltid=AfmBOor6NQO7HSF1h1JLWIri1FpM–K2ZVnrSJXb33SznRSSX8UJZwAi
[7] – https://www.onedose.io/en/how-to-measure-insulin-resistance-at-home/
[8] – https://www.healthline.com/health/diabetes/insulin-resistance-symptoms
[9] – https://www.medicalnewstoday.com/articles/305567
[10] – https://www.rupahealth.com/post/insulin-resistance-testing
[11] – https://www.rupahealth.com/post/reverse-insulin-resistance
[12] – https://www.eatingwell.com/article/8072847/7-day-weight-loss-meal-plan-for-insulin-resistance/
[13] – https://www.veri.co/learn/insulin-resistance-diet-plan-for-weight-loss?srsltid=AfmBOorJ4bZXEKi6KJ2pL6NTtPhtx51BOfKO4I8hxkRG6iacumBgUN8h
[14] – https://www.healthline.com/nutrition/14-ways-to-lower-insulin
[15] – https://medicine.yale.edu/news-article/how-to-reverse-insulin-resistance/
[16] – https://www.health.com/insulin-resistance-diet-8407040
[17] – https://www.nutrisense.io/blog/meal-frequency-and-insulin-sensitivity?srsltid=AfmBOooVCVBC_fi7uc3Xwmxr2BeXv5ugLFv4oXgrouLn49h9lPFqvtmo
[18] – https://pmc.ncbi.nlm.nih.gov/articles/PMC10903815/
[19] – https://www.nature.com/articles/ijo2017199
[20] – https://zoe.com/learn/insulin-resistance-diet
[21] – https://pmc.ncbi.nlm.nih.gov/articles/PMC6509938/
[22] – https://pmc.ncbi.nlm.nih.gov/articles/PMC3671133/
[23] – https://www.quora.com/Is-it-possible-to-reverse-insulin-resistance-without-exercise
[24] – https://diabetesjournals.org/care/article/26/11/2977/22255/Effective-Exercise-Modality-to-Reduce-Insulin
[25] – https://www.clinicaladvisor.com/features/prescribing-exercise-insulin-resistance-diabetes/
[26] – https://pmc.ncbi.nlm.nih.gov/articles/PMC8971350/
[27] – https://www.healthline.com/nutrition/improve-insulin-sensitivity
[28] – https://vitalityhealthmatrix.com/understanding-the-connection-between-stress-and-insulin-resistance/
[29] – https://www.medicalnewstoday.com/articles/323027
[30] – https://www.sciencedirect.com/science/article/pii/S0147651323014136
[31] – https://pmc.ncbi.nlm.nih.gov/articles/PMC5788318/
[32] – https://diabetesjournals.org/spectrum/article/15/2/109/459/Toxins-and-Diabetes-Mellitus-An-Environmental
[33] – https://emedicine.medscape.com/article/122501-medication
[34] – https://pmc.ncbi.nlm.nih.gov/articles/PMC9182772/
[35] – https://www.verywellhealth.com/options-for-treating-insulin-resistance-2616669
[36] – https://my.clevelandclinic.org/health/diseases/22206-insulin-resistance
[37] – https://pmc.ncbi.nlm.nih.gov/articles/PMC8836112/
[38] – https://emedicine.medscape.com/article/122501-treatment
[39] – https://drc.bmj.com/content/7/1/e000723
[40] – https://onlinelibrary.wiley.com/doi/10.1111/1753-0407.12443
[41] – https://pmc.ncbi.nlm.nih.gov/articles/PMC8828446/